Maintaining stable blood sugar levels is not only important for people with diabetes but also for those without the condition. Even if you do not have diabetes, your blood sugar still plays a vital role in energy regulation, sleep quality, and long-term metabolic health. Bedtime is a particularly important moment to consider because your body continues to use glucose throughout the night, fueling the brain and essential organs. Understanding what your blood sugar should be at bedtime can help you maintain overall well-being and reduce the risk of developing future health issues.
This article explores in detail what normal blood sugar levels look like before sleep, factors that influence glucose regulation at night, and tips for maintaining healthy levels without diabetes. By the end, you will have a comprehensive view of how to support your body’s natural rhythms and achieve balanced blood sugar.
Understanding Blood Sugar in People Without Diabetes
Blood sugar, also called blood glucose, refers to the amount of glucose circulating in your bloodstream. Glucose comes primarily from carbohydrates in food and serves as your body’s main source of energy. For people without diabetes, the body tightly regulates blood sugar levels using insulin and other hormones to keep them within a healthy range.
During the day, blood sugar fluctuates in response to meals, physical activity, and stress. At night, however, your body continues to regulate blood sugar in a slightly different way. The liver releases small amounts of glucose to ensure your brain and muscles receive steady fuel while you sleep. Hormones like cortisol and growth hormone also influence nighttime glucose patterns, meaning bedtime levels are especially significant.
If you do not have diabetes, your body typically keeps glucose within a safe window. Still, bedtime readings can reveal important information about your metabolism, dietary habits, and overall health.
Normal Blood Sugar Ranges at Bedtime Without Diabetes
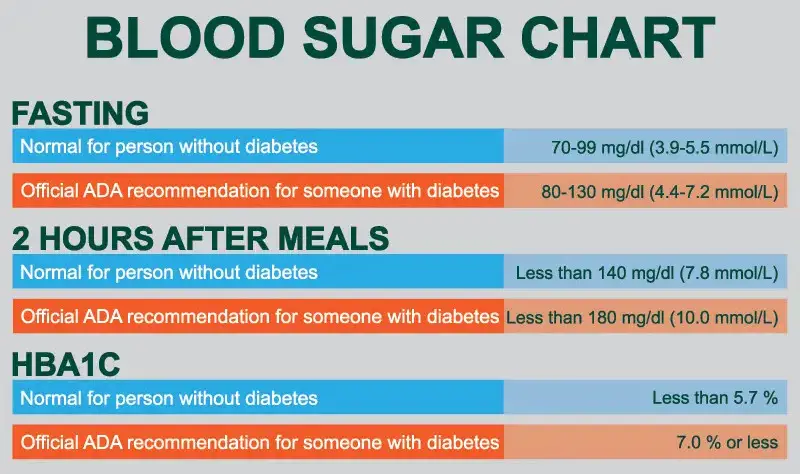
For individuals without diabetes, fasting blood sugar usually ranges between 70 and 99 mg/dL. However, bedtime levels are slightly different since you have recently eaten or are in the process of digesting dinner. In most cases, a normal bedtime blood sugar for a non-diabetic adult falls between 90 and 120 mg/dL.
If your blood sugar is on the lower end of this spectrum, your body is likely processing glucose efficiently and maintaining balance. If it is slightly higher, it may reflect your most recent meal or natural hormonal fluctuations before sleep. These numbers can shift depending on age, activity level, stress, and even genetics.
A bedtime blood sugar consistently outside this range could be an early sign of insulin resistance or other metabolic issues. Although occasional fluctuations are normal, persistent high or low readings may warrant lifestyle adjustments and consultation with a healthcare professional.
Why Bedtime Blood Sugar Matters
Bedtime blood sugar provides insight into how well your body is managing glucose throughout the day. Going to bed with balanced glucose can improve sleep quality, reduce nighttime awakenings, and prevent feelings of hunger that may disrupt rest. In contrast, very low or very high bedtime glucose can cause problems.
Low blood sugar at night may lead to restless sleep, vivid dreams, or even waking up with headaches. On the other hand, elevated bedtime glucose can interfere with deep sleep cycles and leave you feeling tired the next morning. Over time, frequent spikes in nighttime blood sugar—even in people without diabetes—can increase the risk of weight gain, metabolic syndrome, and prediabetes.
By monitoring and understanding your bedtime blood sugar, you gain valuable feedback about your diet, physical activity, and stress levels. This knowledge empowers you to make small adjustments that support long-term health.
Factors That Influence Bedtime Blood Sugar Without Diabetes
Even if you do not have diabetes, many factors can affect your blood sugar at night. These influences often work together, making each evening reading slightly different.
The Role of Diet and Evening Meals
Your last meal of the day plays a central role in determining bedtime blood sugar. Meals high in refined carbohydrates, such as white bread or sugary desserts, can cause temporary spikes that last into the night. Balanced meals with protein, fiber, and healthy fats tend to result in steadier readings.
Timing also matters. Eating a large meal too close to bedtime can keep blood sugar elevated while you are trying to fall asleep. A lighter meal eaten earlier in the evening usually allows your body enough time to process glucose before rest.
Physical Activity and Daily Movement
Exercise affects how your muscles use glucose, often lowering blood sugar levels for several hours. If you have been active during the day, your bedtime readings may be lower and more stable. On the other hand, a sedentary day can lead to slightly higher bedtime glucose. Evening workouts, particularly those involving moderate activity like walking, may help regulate bedtime levels without causing dramatic drops.
Stress and Hormonal Influence
Stress triggers the release of cortisol and adrenaline, both of which can raise blood sugar temporarily. If you go to bed feeling anxious or after a stressful evening, your bedtime glucose might be higher than usual. Similarly, natural hormonal rhythms that occur at night can influence how much glucose your liver releases, leading to small variations in readings.
Alcohol and Caffeine Intake
Alcohol can lower blood sugar by interfering with the liver’s ability to release glucose, sometimes resulting in drops during the night. Caffeine, on the other hand, may raise glucose slightly in some people. If consumed in the evening, both can have noticeable effects on bedtime levels.
Sleep Patterns and Circadian Rhythm
Your body’s internal clock influences how hormones like insulin and cortisol function. Poor or irregular sleep can disrupt these patterns, leading to inconsistent glucose control. Going to bed and waking up at consistent times can help stabilize both your sleep and your blood sugar.
The Relationship Between Bedtime Blood Sugar and Sleep Quality
Blood sugar stability is closely tied to sleep quality. When glucose remains within a healthy range at bedtime, your body is more likely to transition smoothly into restorative sleep. Stable blood sugar also reduces the risk of waking up hungry or experiencing night sweats and restlessness.
Conversely, blood sugar dips or spikes at night can disrupt the sleep cycle. A rapid drop in glucose may trigger adrenaline release, causing you to wake up suddenly. High glucose may prevent your body from entering deep sleep stages, leaving you groggy in the morning. Over time, disrupted sleep and poor glucose control can reinforce each other, creating a cycle that affects both energy and health.
Maintaining balanced blood sugar at bedtime therefore supports not only metabolic health but also restorative sleep.
Long-Term Health Implications of Bedtime Blood Sugar
Although a single bedtime reading may not mean much on its own, consistent patterns reveal important information about your long-term health. Persistently high readings, even without diabetes, may signal insulin resistance, a condition in which your body’s cells respond less effectively to insulin. This can increase the risk of prediabetes, type 2 diabetes, and cardiovascular issues.
On the other hand, frequent low readings may indicate issues with nutrition or hormone regulation. For example, skipping meals or consuming too little carbohydrate can lead to dips in blood sugar, which may cause fatigue and other symptoms over time.
Monitoring bedtime glucose can therefore serve as an early warning system, helping you make lifestyle changes before problems develop.
Tips for Maintaining Healthy Bedtime Blood Sugar Without Diabetes
Achieving balanced bedtime blood sugar without diabetes involves supporting your body’s natural ability to regulate glucose. While everyone’s body responds differently, several strategies tend to promote stability.
Focus on Balanced Evening Meals
Choose dinners that include lean proteins, whole grains, vegetables, and healthy fats. This combination slows digestion and prevents sharp spikes in blood sugar. Avoid heavy desserts or processed snacks close to bedtime, as these can elevate glucose for hours.
Keep a Consistent Eating Schedule
Going too long without food during the day may cause blood sugar to drop, while late-night eating can keep levels high at bedtime. Aim for a routine where your last meal is finished at least two to three hours before sleep. This gives your body time to process glucose before rest.
Incorporate Gentle Evening Activity
Light movement after dinner, such as a short walk, can help your muscles absorb glucose and bring levels into a healthier range. Gentle stretching or yoga may also improve relaxation and indirectly benefit glucose stability by lowering stress.
Manage Stress Before Bed
Relaxation techniques such as deep breathing, meditation, or reading can lower stress hormones that otherwise raise blood sugar. Creating a calming bedtime routine helps not only your glucose but also your overall sleep quality.
Prioritize Quality Sleep
Getting seven to nine hours of sleep each night supports balanced hormone function, including insulin sensitivity. Poor sleep or irregular sleep schedules may raise glucose levels even in people without diabetes.
Stay Hydrated
Proper hydration helps your body regulate blood sugar more efficiently. Drinking enough water throughout the day ensures your body can transport and balance glucose effectively.
When to Be Concerned About Bedtime Blood Sugar
For most people without diabetes, small variations in bedtime blood sugar are normal. However, there are circumstances where readings may warrant closer attention. Consistently high readings above 130–140 mg/dL at bedtime, especially if accompanied by fatigue or increased thirst, may indicate developing insulin resistance. Repeatedly low readings below 70 mg/dL may suggest dietary imbalances or other underlying issues.
If you notice persistent patterns outside the normal range, it may be helpful to discuss them with a healthcare provider. While occasional fluctuations are expected, ongoing irregularities can point to early stages of metabolic dysfunction. Testing blood sugar occasionally at bedtime and in the morning can provide a fuller picture of how your body is managing glucose.
The Connection Between Bedtime Blood Sugar and Prediabetes Risk
Prediabetes often develops silently over time, with only subtle changes in blood sugar regulation. Bedtime readings that tend to run higher than normal may be one of the earliest signs. Although not a diagnostic tool on their own, these numbers can reveal whether your body is beginning to struggle with glucose management.
Taking action early by improving diet, increasing physical activity, and reducing stress can reverse prediabetes in many cases. Therefore, paying attention to bedtime blood sugar without diabetes not only supports daily well-being but also provides a safeguard against long-term risks.
Practical Ways to Check Bedtime Blood Sugar Without Diabetes
People without diabetes are not usually required to check their blood sugar, but some choose to do so for health awareness. Home glucose meters, which require a small finger-prick sample, provide quick readings. Continuous glucose monitors are another option, offering real-time insights into how meals and activities affect glucose throughout the day.
Occasional bedtime checks can help you understand how your body responds to different foods, stress levels, or exercise routines. This knowledge allows you to tailor your lifestyle to support more consistent glucose balance, even if you do not have diabetes.
Conclusion
Blood sugar at bedtime plays a crucial role in health, even for individuals without diabetes. A normal range of about 90 to 120 mg/dL reflects your body’s ability to regulate glucose effectively during the day and prepare for restorative sleep. Multiple factors—from diet and exercise to stress and sleep patterns—shape bedtime readings, and small variations are expected.
By paying attention to your body’s signals and supporting healthy routines, you can keep bedtime glucose within an optimal range. Doing so not only improves sleep quality and daily energy but also protects long-term metabolic health. Monitoring and maintaining balanced bedtime blood sugar is therefore a valuable practice for anyone who wishes to stay healthy and prevent future complications.
FAQs About Bedtime Blood Sugar Without Diabetes
What is the ideal blood sugar before bed if I don’t have diabetes?
For most healthy adults without diabetes, the ideal blood sugar range at bedtime is between 90 and 120 mg/dL. This range supports stable overnight energy and restorative sleep. Slight variations are normal depending on your last meal, activity, and stress levels.
Can high bedtime blood sugar mean I have diabetes?
Not necessarily. A single high reading does not mean you have diabetes. Blood sugar naturally rises after meals, and bedtime values can be temporarily elevated. However, consistently high readings above 130–140 mg/dL at night may suggest early insulin resistance or prediabetes, and you should consider speaking with a healthcare provider.
Does eating late at night affect blood sugar levels?
Yes. Eating a heavy meal or sugary snacks right before bed can keep blood sugar elevated for several hours. This not only affects sleep quality but also increases the likelihood of higher bedtime glucose readings. Finishing your last meal 2–3 hours before bedtime allows your body time to process glucose more effectively.
Can exercise lower my blood sugar before bed?
Moderate activity, such as walking or light stretching after dinner, can help your muscles absorb glucose and bring levels into a healthy range. However, very intense workouts late at night may sometimes raise stress hormones, leading to temporary increases in blood sugar.
Is it dangerous to have low blood sugar before bed without diabetes?
For people without diabetes, low blood sugar before bed is uncommon but can happen if you have not eaten enough during the day or consumed alcohol. Readings below 70 mg/dL may cause restless sleep, hunger, or headaches upon waking. Regularly experiencing low bedtime glucose may indicate dietary imbalances.
Should I check my blood sugar at bedtime if I don’t have diabetes?
Routine checks are not necessary for most people without diabetes. However, using a home glucose meter or continuous glucose monitor occasionally can provide insight into how your body responds to food, stress, or activity. This can be especially useful if you have risk factors for prediabetes or metabolic syndrome.
How does bedtime blood sugar relate to prediabetes risk?
Bedtime readings that consistently trend high may be one of the earliest signs of prediabetes. While not diagnostic, these patterns indicate your body may be struggling with insulin sensitivity. Early lifestyle changes—such as improved diet, exercise, and stress management—can often reverse prediabetes before it develops into diabetes.
Disclaimer: This article is intended for informational purposes only and should not be taken as medical advice. Blood sugar levels vary from person to person, and what is normal for one individual may differ for another. If you are concerned about your bedtime blood sugar or notice consistent irregularities, consult with a qualified healthcare professional for personalized guidance.
References
- Centers for Disease Control and Prevention (CDC) – Diabetes and Blood Sugar
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Checking Blood Sugar
- MedlinePlus (U.S. National Library of Medicine) – Blood Glucose