Quick answer: Ozempic (semaglutide) is not insulin—it’s a once-weekly GLP-1 receptor agonist for Type 2 diabetes, while insulin is essential for Type 1 diabetes and often needed in advanced Type 2. Many patients use both together—a GLP-1 RA plus basal insulin—under a clinician’s plan to reach A1C goals with fewer hypoglycemic events. Always follow your own clinician’s advice and FDA-approved labeling.
The GLP-1 receptor is a G protein–coupled receptor (GPCR) activated by the incretin hormone glucagon-like peptide-1 (GLP-1) and is expressed on cell surfaces throughout the body—most notably in the pancreatic β-cells, brain, and gut—where its activation supports glucose-dependent insulin secretion, tempers glucagon release, increases satiety, and slows gastric emptying to improve post-meal control; because these coordinated effects lower blood glucose and help with appetite regulation, the GLP-1 receptor has become a cornerstone therapeutic target in Type 2 diabetes and obesity, guiding the development of GLP-1 receptor agonists used under clinician supervision for long-term metabolic management.
What is Ozempic?
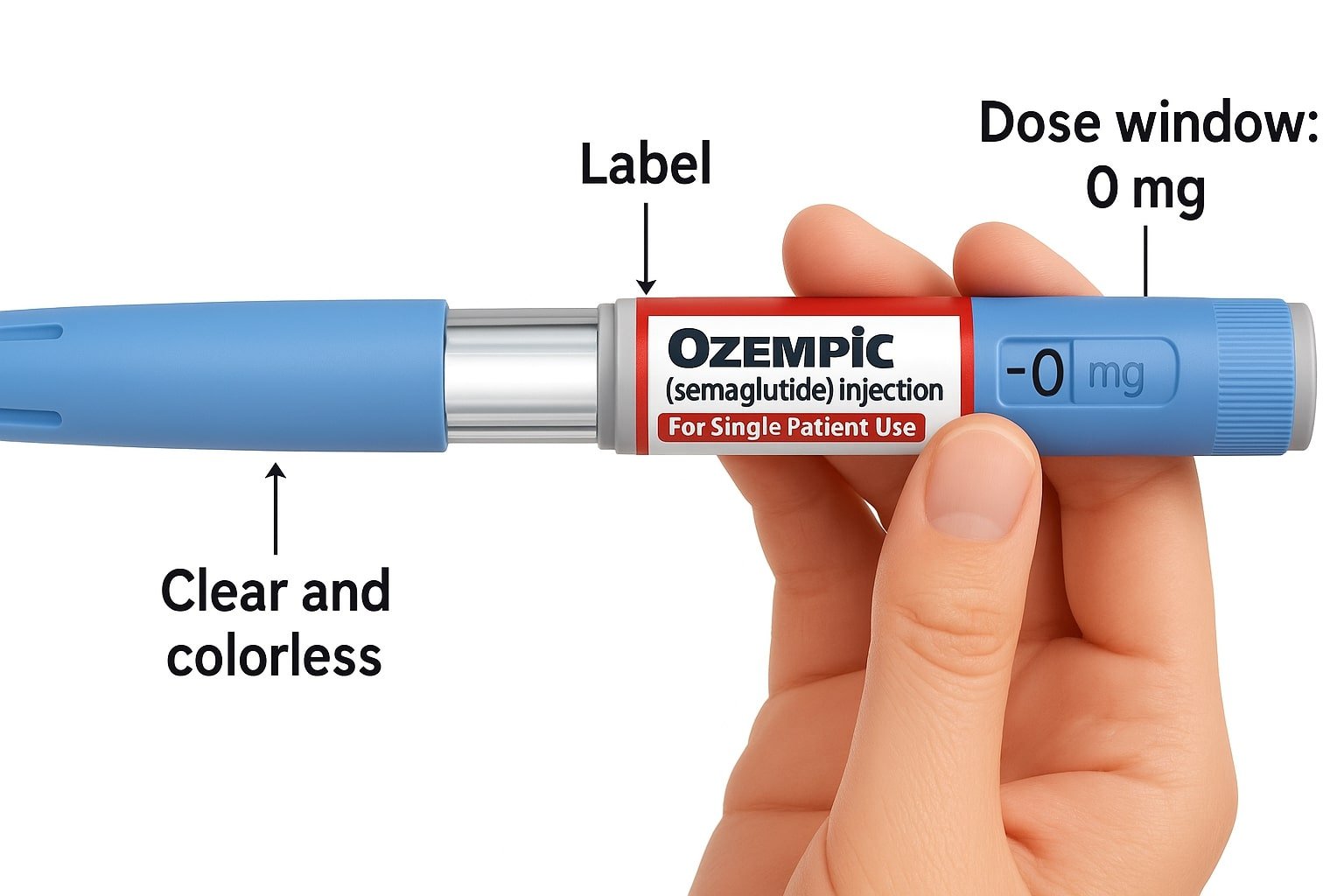
Ozempic is the brand name for semaglutide, a prescription GLP-1 receptor agonist given as a once-weekly under-the-skin injection for adults with type 2 diabetes. It helps lower blood sugar and, in adults with type 2 diabetes who already have heart disease, it is also used to reduce the risk of major cardiovascular events. Ozempic is not insulin and does not replace insulin in type 1 diabetes or during diabetic ketoacidosis.
How it works:
it enhances insulin release only when glucose is high, reduces glucagon, and slows stomach emptying. These actions can improve after-meal control and often lead to reduced appetite and weight loss.
Typical dosing (your clinician sets the plan): start at 0.25 mg once weekly for 4 weeks, then 0.5 mg; maintenance doses range from 0.5 mg to 2 mg once weekly based on response and tolerance.
Common side effects
Common side effects include nausea, vomiting, diarrhea, and constipation; it can also cause gallbladder issues and dehydration-related kidney problems. Serious but uncommon risks include pancreatitis and, per a boxed warning, thyroid C-cell tumors—do not use if you or a family member has had medullary thyroid carcinoma or MEN2. Always use Ozempic only under a clinician’s guidance and follow the approved labeling for safe use.
What each medicine is—and how it works
Insulin replaces or supplements the body’s insulin to directly lower blood glucose. Basal options (e.g., insulin glargine) provide steady 24-hour coverage, and mealtime insulin may be added for post-meal spikes. The primary risk is hypoglycemia, so dose, meal timing, and activity need careful coordination.
Ozempic (semaglutide) is a GLP-1 receptor agonist: it enhances glucose-dependent insulin secretion, slows gastric emptying, and reduces hepatic glucose output. It’s once weekly and often supports weight loss as part of a comprehensive plan.
Who typically uses which?
- Type 1 diabetes (T1D): Insulin is non-negotiable; GLP-1 RAs do not replace insulin in T1D.
- Type 2 diabetes (T2D): A GLP-1 RA like Ozempic is considered when oral therapy is insufficient or when weight and cardiometabolic goals are priorities. Insulin is introduced when hyperglycemia is more severe, rapid control is needed, or other agents are inadequate.
Can you use them together?
Yes. Many T2D regimens combine a GLP-1 RA with basal insulin to improve A1C while limiting hypoglycemia and weight gain compared with escalating mealtime insulin alone. Doses are individualized and titrated gradually; do not change your doses without professional guidance.
Safety essentials (read before starting)
- Ozempic: Common GI symptoms (nausea, vomiting). Boxed warning for thyroid C-cell tumors; do not use if there’s a personal/family history of MTC or MEN2. Seek care urgently for severe abdominal pain that could signal pancreatitis.
- Insulin: Main risk is hypoglycemia (shakiness, confusion, sweating; severe cases can be dangerous). Keep fast-acting carbohydrates available and review dose adjustments for meals, activity, illness, and travel.
Comparison table (accessible, source-ready)
| Feature | Ozempic | Basal insulin |
|---|---|---|
| Medication class | GLP-1 receptor agonist | Long-acting insulin analogue |
| Primary use | **Type 2 diabetes**; weekly dosing; weight & cardio-metabolic considerations | **Type 1 & Type 2 diabetes** to improve glycemic control |
| How it works | Boosts insulin **when glucose is high**, slows gastric emptying | Directly lowers glucose via steady background insulin |
| Key benefits | Glucose control with **weight-loss support** in many T2D patients | Essential for **T1D**; titratable and reliable glucose lowering |
| Main risks | GI effects; **boxed warning** for thyroid C-cell tumors; pancreatitis risk | **Hypoglycemia**; potential weight gain |
| When combined | Often **GLP-1 RA + basal insulin** in T2D to reach A1C targets with fewer hypos than adding mealtime insulin | |
| Dosing rhythm | **Once weekly** injection | **Daily** (time-consistent) injection |
Weight & daily life (realistic expectations)
Insulin therapy can be associated with weight gain as glucose control improves; careful dose optimization, meal planning, and activity help. GLP-1 therapy commonly supports weight reduction and reduced appetite, but results vary and depend on consistent SMBG/CGM use, adherence, and lifestyle.
Costs & access (U.S. context)
Out-of-pocket costs differ by insurance, dose, pharmacy, and eligibility for savings programs. Rather than quoting static prices, verify formulary status, any step-therapy rules, and current support options with your clinician or pharmacist. Always date your price notes for accuracy.
FAQs: Ozempic vs Insulin
Is Ozempic better than insulin?
They serve different roles. Insulin is essential for Type 1 diabetes and often required in advanced Type 2. Ozempic (semaglutide) is a GLP-1 receptor agonist for Type 2 that may support weight reduction and post-meal control when appropriate. Many patients use both together—a GLP-1 RA plus basal insulin—under clinician guidance.
Can Ozempic replace insulin?
No for Type 1. In Type 2, Ozempic may reduce insulin needs, but any change must be clinician-directed. Never start, stop, or switch therapies without a personalized plan.
Does insulin cause weight gain?
Possible. Improved glucose uptake with insulin can increase weight in some users. Strategies include dose optimization, meal planning, activity adjustments, and close review of logs (SMBG/CGM) with your care team.
What insulin is comparable to Ozempic?
None. Ozempic is a GLP-1 RA, not insulin. Basal insulin provides steady background insulin to directly lower glucose; it addresses a different clinical need.
How much weight can you lose with Ozempic?
Results vary by dose, adherence, and individual factors. Many people with Type 2 see meaningful weight reduction when Ozempic is used as prescribed alongside nutrition, activity, and monitoring.
What A1C qualifies for Ozempic?
Use is individualized. Clinicians consider diagnosis, A1C goals, current medications, cardio-renal risks, and tolerance—not a single cutoff. Ask how a GLP-1 RA fits your plan.
Educational only: No individual medical care is provided here. Always follow your clinician’s advice and FDA-approved labeling.
NOTE: Educational content only; no individual medical care is provided here. Always follow your own clinician’s advice and FDA-approved labeling, and never start, stop, or combine medications without professional guidance.
Reference notes (for your internal review only — do not publish on the page)
- ADA Standards of Care 2025 for pharmacologic pathways, GLP-1 RA roles, and insulin use. (Diabetes Journals, PubMed, American Diabetes Association)
- Ozempic (semaglutide) FDA label (2025) for boxed warning, contraindications (MTC/MEN2), and weekly dosing. (FDA Access Data)
- Insulin glargine (Lantus) FDA label for indication and hypoglycemia risk. (FDA Access Data)
- Evidence supporting GLP-1 RA + basal insulin combinations improving A1C with less hypoglycemia/weight gain. (Diabetes Journals, PubMed, BioMed Central, wafp.org)