Managing diabetes effectively depends on precise insulin dosing, and insulin lispro—a rapid-acting insulin analog—plays a vital role in controlling blood sugar levels after meals. Determining the right insulin lispro dosage is essential for preventing both hyperglycemia and hypoglycemia.
This guide provides a comprehensive look at insulin lispro, including how it works, how dosages are determined, and key factors that influence dosing requirements. Whether you’re newly prescribed this insulin or looking to optimize your current regimen, understanding dosage principles can help you stay safe and in control.
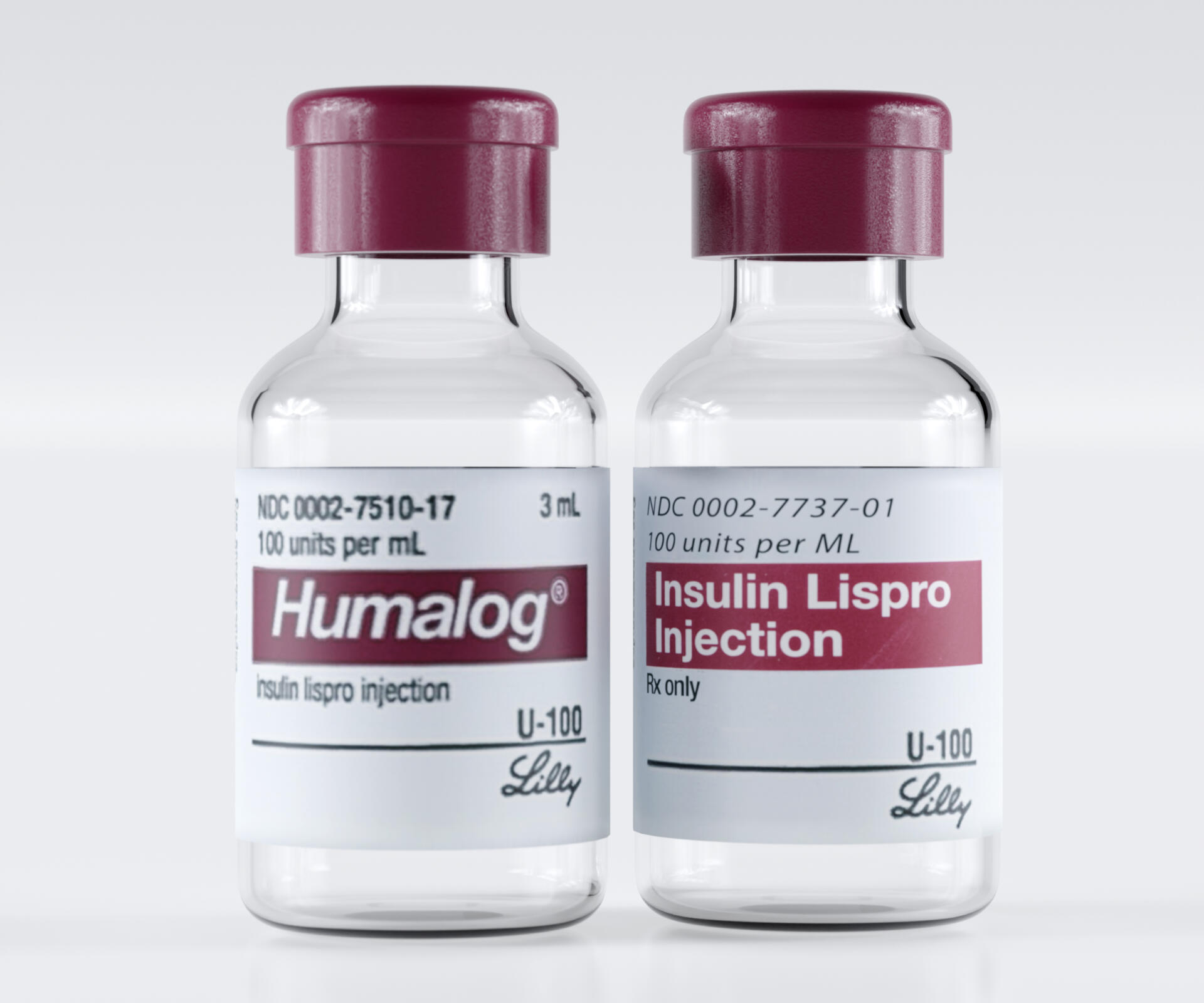
What Is Insulin Lispro?

Insulin lispro is a fast-acting synthetic insulin designed to mimic the natural insulin response of the body after eating. It begins working within 10 to 20 minutes, peaks around 1 hour, and typically lasts for about 3 to 5 hours.
It’s often sold under brand names such as Humalog, Admelog, and Lyumjev, and is used by both Type 1 and Type 2 diabetic patients. Its rapid onset helps lower post-meal glucose spikes, making it ideal for use right before or immediately after meals.
Because of its quick action, dosing must be precise and well-timed, depending on your blood sugar level, carbohydrate intake, and overall insulin plan.
How Insulin Lispro Works in the Body
Insulin lispro functions by facilitating glucose uptake into the body’s cells and preventing the liver from producing excess glucose. It closely imitates the body’s normal insulin response following a meal.
Unlike long-acting insulins that provide a steady baseline, rapid-acting insulins like lispro target the sharp rise in blood sugar caused by food. This means timing and dosage are crucial—injecting too early or too much may lead to dangerously low blood sugar.
Understanding how your body responds to different foods and daily routines helps your healthcare provider fine-tune your insulin lispro dosage.
Typical Starting Dosage for Insulin Lispro
For Type 1 Diabetes
For individuals with Type 1 diabetes, the total daily insulin dose (TDD) generally ranges between 0.4 and 1.0 units per kilogram of body weight. About half of this total is usually given as basal insulin, while the other half is divided among meals as bolus insulin, which includes insulin lispro.
For example, a 70 kg adult might need a total of 28 to 70 units per day. Around 14 to 35 units of this total would be covered by insulin lispro, distributed across meals based on carbohydrate intake and blood sugar levels.
For Type 2 Diabetes
For Type 2 diabetes, insulin lispro may be added to oral medications or long-acting insulin if post-meal glucose control is insufficient. Starting doses are typically 4 to 6 units before the largest meal, with gradual adjustments based on blood sugar readings.
Some patients may require pre-meal injections before breakfast, lunch, and dinner, depending on glucose response and medical advice.
Factors That Affect Insulin Lispro Dosage
Insulin dosage is never one-size-fits-all. It varies based on personal metabolic factors, activity levels, and diet. Below are the main influences on insulin lispro requirements.
1. Carbohydrate Intake
Carbohydrates directly raise blood glucose levels, so the amount of insulin lispro needed before each meal depends on the grams of carbs consumed. The carb-to-insulin ratio (CIR) helps calculate the correct dose—typically 1 unit of insulin per 10 to 15 grams of carbs, though this ratio can vary widely.
2. Blood Sugar Levels Before Meals
Pre-meal glucose readings help determine correction doses. If blood sugar is already elevated before eating, an additional small dose (correction factor) may be added to bring levels into the target range.
3. Physical Activity
Exercise increases insulin sensitivity, meaning you may require less insulin after or before physical activity. Monitoring glucose closely after workouts helps prevent hypoglycemia.
4. Stress and Illness
Stress hormones like cortisol raise blood glucose, requiring temporary dosage increases. Likewise, infections or illnesses may affect insulin needs.
5. Time of Day
Some people experience dawn phenomenon, where blood sugar rises early in the morning. Adjustments in morning insulin lispro doses may help counteract this.
6. Type of Insulin Regimen
Your dosage also depends on whether you’re using multiple daily injections (MDI) or an insulin pump. Pumps deliver lispro in smaller, controlled doses throughout the day.
How to Calculate Your Insulin Lispro Dose
Determining the correct insulin lispro dose involves two major components: meal coverage and correction factor.
Carbohydrate Coverage Dose
The carb ratio tells you how many grams of carbohydrates are covered by one unit of insulin. For instance, if your ratio is 1:12, and you plan to eat 60 grams of carbs, you’d take 5 units (60 ÷ 12).
Correction Dose
This is used when blood sugar is above target levels before a meal. The correction factor (or insulin sensitivity factor, ISF) indicates how much one unit of insulin lowers your blood sugar.
For example, if your ISF is 50, and your current glucose is 200 mg/dL with a target of 120 mg/dL, you need:
(200 – 120) ÷ 50 = 1.6 units, rounded to 2 units.
When combined, you would inject the total of the meal dose and correction dose.
When and How to Take Insulin Lispro
Timing of Injection
Because insulin lispro acts quickly, it’s generally injected within 15 minutes before a meal, or even right after eating in some cases. Injecting too early can cause low blood sugar before food is absorbed, while injecting too late may lead to high post-meal glucose.
Injection Sites
Common injection sites include the abdomen, thighs, buttocks, and upper arms. The abdomen is often preferred for the fastest absorption.
Rotation of Sites
Always rotate injection spots to avoid lipohypertrophy (fatty lumps that slow insulin absorption).
Storage
Unopened insulin lispro should be kept in the refrigerator, while opened vials or pens can typically be stored at room temperature (below 86°F / 30°C) for up to 28 days.
Monitoring Blood Glucose and Adjusting Dosage
Close monitoring is essential for accurate insulin lispro dosing. Using continuous glucose monitors (CGMs) or frequent finger-stick tests helps identify trends and prevent hypo- or hyperglycemia.
Your healthcare provider may adjust your insulin lispro dosage weekly or biweekly based on these readings. Always track your results in a logbook or diabetes management app for pattern recognition.
Never adjust insulin dosages drastically on your own. Even small changes should be made cautiously and under medical supervision.
Possible Side Effects of Incorrect Dosing
Incorrect dosing of insulin lispro can cause potentially serious side effects.
Hypoglycemia (Low Blood Sugar)
The most common side effect of taking too much insulin. Symptoms include sweating, shaking, confusion, dizziness, and in severe cases, unconsciousness. Consuming glucose tablets or sugary foods immediately helps reverse mild hypoglycemia.
Hyperglycemia (High Blood Sugar)
Too little insulin leads to high blood sugar, resulting in thirst, frequent urination, fatigue, and blurred vision. Persistent hyperglycemia can lead to diabetic ketoacidosis (DKA).
Injection Site Reactions
Mild redness or swelling can occur. Rotating sites and using clean needles help reduce this risk.
Allergic Reactions
Rarely, individuals may experience allergic responses. Seek immediate medical attention if severe itching, rash, or swelling develops.
Differences Between Insulin Lispro and Other Rapid-Acting Insulins
Insulin lispro is similar to insulin aspart (NovoLog) and insulin glulisine (Apidra) in speed and duration. However, lispro is known for slightly faster onset and flexible timing.
Insulin Lispro vs. Regular Human Insulin
Regular insulin takes longer to act (30–60 minutes), while lispro starts working within 15 minutes, providing better post-meal glucose control. This means fewer blood sugar spikes and more freedom in mealtime scheduling.
Insulin Lispro vs. Long-Acting Insulin
Long-acting insulins like glargine or detemir provide steady baseline coverage, not rapid correction. Lispro is used specifically for meals or rapid correction of high glucose.
Combining both types creates a basal-bolus regimen, offering precise and balanced glucose management throughout the day.
Practical Tips for Safe Insulin Lispro Use
- Always check insulin appearance before use; it should be clear and colorless.
- Avoid mixing lispro with other insulins unless directed by your healthcare provider.
- Carry glucose tablets in case of unexpected low blood sugar.
- Record your doses and timing consistently to identify response patterns.
- Travel with backup insulin and keep it at proper storage temperature.
These habits ensure stable glucose control and prevent potentially dangerous fluctuations.
When to Consult Your Healthcare Provider
Always consult your doctor or diabetes educator if you experience frequent hypoglycemia, unexplained glucose variability, or if your diet or activity levels change significantly.
You may also need a dosage reassessment during:
- Illness or infection
- Pregnancy
- Weight changes
- Starting or stopping medications that affect blood sugar (like steroids)
A healthcare professional can help recalculate your insulin-to-carb ratio or correction factor for safe adjustment.
Special Considerations for Children and the Elderly
Children
Children typically have higher insulin sensitivity, so their insulin lispro doses are smaller and must be adjusted carefully. Pediatric dosing often requires close parental supervision and frequent blood glucose monitoring.
Elderly Patients
Older adults may have slower metabolism or kidney function changes, affecting insulin clearance. Lower starting doses are often recommended to minimize hypoglycemia risk.
Both age groups require individualized care and medical oversight.
Future of Insulin Lispro and Smart Dosing
With advancements in smart insulin pens and automated insulin pumps, managing insulin lispro dosage is becoming more precise and user-friendly. These devices calculate doses automatically based on real-time glucose data, reducing guesswork and human error.
Additionally, AI-based glucose monitoring apps and continuous insulin delivery systems are improving treatment outcomes for people using insulin lispro worldwide.
FAQs About Insulin Lispro Dosage
Below are some of the most frequently asked questions about insulin lispro dosage, timing, and safety. These answers will help you better understand how to use this fast-acting insulin effectively and confidently.
How do I know the right insulin lispro dosage for me?
Your correct insulin lispro dosage depends on several factors, including your body weight, carbohydrate intake, pre-meal blood glucose, and overall insulin sensitivity. Typically, doctors start you on a personalized dose based on your total daily insulin requirement, then fine-tune it using blood sugar monitoring results. Never self-adjust large dose changes without consulting your healthcare provider.
When should I inject insulin lispro?
Insulin lispro should be injected within 15 minutes before eating or right after a meal, depending on your blood sugar level and physician’s advice. Injecting too early can lead to low blood sugar, while taking it too late may result in a post-meal glucose spike. The key is to match insulin action with your meal timing.
Can insulin lispro be mixed with other insulins?
In most cases, insulin lispro should not be mixed with other types of insulin unless specifically directed by your healthcare provider. Some premixed versions, such as Humalog Mix 75/25, are designed for convenience, but mixing manually can alter absorption rates and reduce safety. Always check the label or ask your doctor before combining insulins.
What happens if I take too much insulin lispro?
Taking too much insulin lispro can cause hypoglycemia (low blood sugar). Symptoms include trembling, dizziness, sweating, confusion, and, in severe cases, fainting or seizures. If this happens, immediately consume fast-acting carbohydrates such as glucose tablets, juice, or regular soda, and seek medical help if symptoms don’t improve quickly.
Can I skip a dose of insulin lispro if I don’t eat?
If you skip a meal, it’s usually safe to skip your mealtime insulin lispro dose as well, since this insulin is meant to control post-meal glucose spikes. However, never skip your long-acting insulin (if prescribed), as it maintains baseline glucose levels. Always confirm with your healthcare provider for your specific regimen.
How long does insulin lispro last in the body?
Insulin lispro begins to work within 10–20 minutes, peaks around 1 hour, and typically lasts for 3–5 hours. Because of its short duration, it’s mainly used to manage glucose levels after meals rather than as a basal insulin.
What should I do if my blood sugar remains high after taking insulin lispro?
If your blood sugar remains high after dosing, double-check your carb counting, injection timing, and insulin storage conditions. Sometimes insulin may lose potency if exposed to heat or freezing. If high blood sugar persists, consult your doctor to adjust your carb ratio or correction factor appropriately.
Can I use insulin lispro in an insulin pump?
Yes, insulin lispro is approved for use in insulin pumps. It works well with continuous subcutaneous insulin infusion (CSII) systems because of its rapid onset and short duration. Pumps can deliver lispro in small, precise doses, offering improved glucose control and flexibility. Ensure your pump settings are verified by your endocrinologist.
What are the side effects of insulin lispro?
Common side effects include mild injection site irritation, hypoglycemia, and occasional swelling or redness. Rarely, allergic reactions or lipodystrophy (thickened skin) may occur. Rotating injection sites and using new needles for each dose can help prevent most issues.
Can insulin lispro go bad if not refrigerated?
Unopened insulin lispro vials or pens should be stored in the refrigerator between 36°F–46°F (2°C–8°C). Once opened, they can be kept at room temperature (below 86°F / 30°C) for up to 28 days. If exposed to heat or direct sunlight, insulin may lose potency—always discard any insulin that appears cloudy or clumpy.
Is insulin lispro safe during pregnancy or breastfeeding?
Insulin lispro is generally considered safe during pregnancy and breastfeeding, as it closely mimics natural human insulin. However, pregnancy can alter insulin requirements, so frequent monitoring and medical supervision are necessary to maintain stable glucose levels and avoid complications.
How do I switch from regular insulin to insulin lispro?
Switching from regular insulin to insulin lispro should only be done under medical supervision. The total daily dose may remain similar, but timing and correction factors often change because lispro acts faster. Your doctor will typically recommend taking lispro 15 minutes before meals, compared to 30 minutes with regular insulin.
Can I travel with insulin lispro?
Yes, but you must store and transport it properly. Keep your insulin in an insulin travel cooler or insulated case to protect it from extreme heat or cold. Carry your insulin lispro in your carry-on luggage rather than checked baggage, and bring a doctor’s note for airport security if you’re flying internationally.
What should I do if I forget my insulin lispro dose?
If you forget to take your dose before a meal, take it as soon as you remember, but only if you’ve eaten recently. If it’s been several hours since your meal, skip that dose and monitor your glucose closely. Avoid taking an extra dose later to “catch up,” as this may cause low blood sugar.
How often should insulin lispro dosage be reviewed?
Your insulin lispro dosage should be reviewed every few weeks or whenever your diet, physical activity, or glucose patterns change significantly. Regular communication with your diabetes care team ensures your dosage remains accurate and safe.
Can insulin lispro cause weight gain?
Like most insulins, insulin lispro can contribute to modest weight gain because it helps the body use glucose more efficiently and reduces glucose loss through urine. Maintaining balanced meals and regular exercise can help minimize this effect.
What’s the difference between Humalog and Admelog?
Both Humalog and Admelog contain insulin lispro and work identically. The main difference lies in their manufacturers and pricing. Admelog is often referred to as a biosimilar version of Humalog and may be more affordable while offering the same effectiveness.
Conclusion
Determining the right insulin lispro dosage is a delicate balance influenced by diet, activity, and individual metabolic needs. It’s not just about following a fixed number of units but learning how your body reacts to meals and daily changes.
By combining professional medical advice, regular glucose monitoring, and informed self-management, you can safely achieve stable blood sugar levels with insulin lispro.
Understanding your insulin regimen empowers you to take charge of your diabetes confidently, ensuring both safety and quality of life every day.
Disclaimer: This article is for educational purposes only and does not substitute professional medical advice. Always consult your healthcare provider for personalized insulin dosing guidance.