1. Introduction
An insulin chart is a tool designed to guide individuals with diabetes in tracking their insulin dosages, timing, and related information. It is widely employed in both clinical and personal settings to address the variability in blood glucose control. By outlining the timing and type of insulin administered, an insulin chart fosters precision and consistency in managing diabetes.
For those in the United States, guidance from the American Diabetes Association (ADA) and the Centers for Disease Control and Prevention (CDC) lays out best practices for medication schedules, dosing, and monitoring. Such practices also intersect with Google’s approach to health content, emphasizing accuracy, transparency, and authoritativeness. By following these considerations, readers can feel more assured about the reliability of the information.
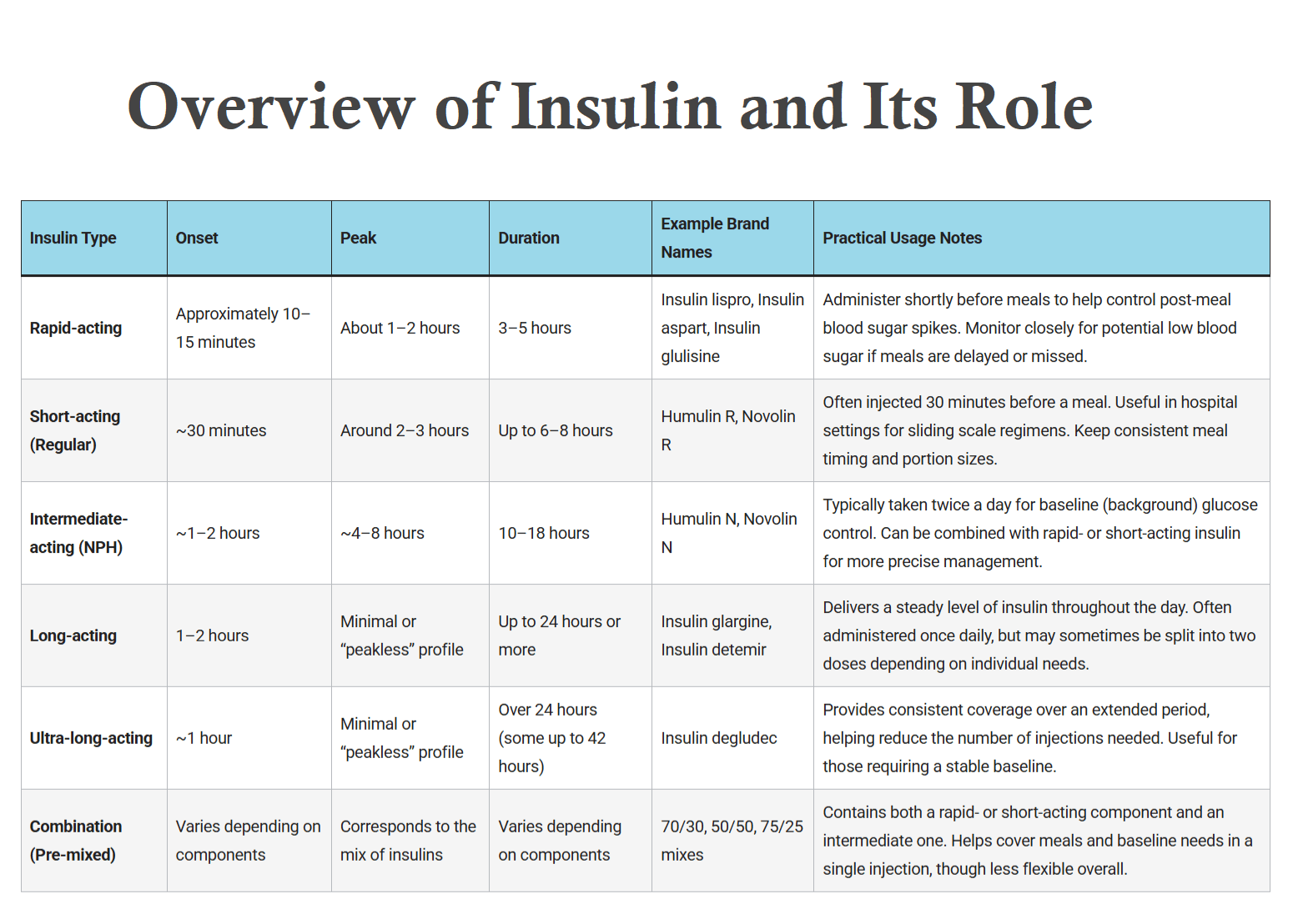
2. Overview of Insulin Chart and Its Role

| Insulin Type | Onset | Peak | Duration | Example Brand Names | Practical Usage Notes |
|---|---|---|---|---|---|
| Rapid-acting | Approximately 10–15 minutes | About 1–2 hours | 3–5 hours | Insulin lispro, Insulin aspart, Insulin glulisine | Administer shortly before meals to help control post-meal blood sugar spikes. Monitor closely for potential low blood sugar if meals are delayed or missed. |
| Short-acting (Regular) | ~30 minutes | Around 2–3 hours | Up to 6–8 hours | Humulin R, Novolin R | Often injected 30 minutes before a meal. Useful in hospital settings for sliding scale regimens. Keep consistent meal timing and portion sizes. |
| Intermediate-acting (NPH) | ~1–2 hours | ~4–8 hours | 10–18 hours | Humulin N, Novolin N | Typically taken twice a day for baseline (background) glucose control. Can be combined with rapid- or short-acting insulin for more precise management. |
| Long-acting | 1–2 hours | Minimal or “peakless” profile | Up to 24 hours or more | Insulin glargine, Insulin detemir | Delivers a steady level of insulin throughout the day. Often administered once daily, but may sometimes be split into two doses depending on individual needs. |
| Ultra-long-acting | ~1 hour | Minimal or “peakless” profile | Over 24 hours (some up to 42 hours) | Insulin degludec | Provides consistent coverage over an extended period, helping reduce the number of injections needed. Useful for those requiring a stable baseline. |
| Combination (Pre-mixed) | Varies depending on components | Corresponds to the mix of insulins | Varies depending on components | 70/30, 50/50, 75/25 mixes | Contains both a rapid- or short-acting component and an intermediate one. Helps cover meals and baseline needs in a single injection, though less flexible overall. |
2.1 Definition and Biological Function
Insulin is a hormone produced by the pancreas, specifically within the beta cells of the islets of Langerhans. Its primary responsibility is to regulate blood glucose levels by promoting the transfer of glucose from the bloodstream into various body cells. When insulin is released, it binds to receptors on cells, initiating processes that help sugar enter the cells, where it can then be used for energy or stored for later use.
Without sufficient insulin activity, glucose cannot effectively enter cells, leading to elevated blood sugar levels. This state, known as hyperglycemia, is the hallmark of diabetes when left unaddressed.
2.2 Natural vs. Synthetic Insulin
- Natural Insulin (Endogenous): The body naturally secretes insulin in response to increases in blood sugar, often triggered by meal intake. This balance is finely controlled by pancreatic cells, adjusting insulin release to keep blood glucose within an optimal range.
- Pharmaceutical (Exogenous) Insulin: Individuals whose bodies do not produce enough insulin or do not efficiently use insulin may require synthetic insulin. Produced through recombinant DNA technology, synthetic versions mimic natural insulin’s function. There are multiple formulations, each with a unique onset, peak, and duration profile to address different clinical needs.
2.3 Mechanism of Action in Blood Sugar Regulation
When food containing carbohydrates is consumed, it is broken down into glucose. This glucose enters the bloodstream and signals the pancreas to secrete insulin. Insulin then interacts with cell receptors, enabling the entry of glucose. In a person without insulin-related problems, this process works smoothly, and blood glucose levels stay within a manageable range.
In diabetes, the balance is disrupted due to either inadequate insulin production, insulin resistance in body tissues, or both. Carefully managed insulin therapy—alongside lifestyle adaptations—helps maintain blood glucose in a safer range.
2.4 Overview of Diabetes Types
- Type 1 Diabetes
- Characterized by an autoimmune process where the body’s immune system attacks the insulin-producing beta cells, resulting in little to no insulin production.
- Individuals commonly require external insulin via injections or an insulin pump.
- Type 2 Diabetes
- Marked by insulin resistance (when cells no longer respond properly to insulin) and/or insufficient insulin production.
- Often managed initially with lifestyle measures and oral medications, though some people may eventually require insulin therapy.
- Gestational Diabetes
- Develops during pregnancy and can affect both maternal and fetal health if not managed appropriately.
- May resolve after childbirth; however, ongoing monitoring is important since it can indicate a higher likelihood of developing Type 2 diabetes later.
Note: Insulin therapy and diabetes management should always be guided by a qualified healthcare professional, considering individual medical history and daily life factors.
3. Types of Insulin
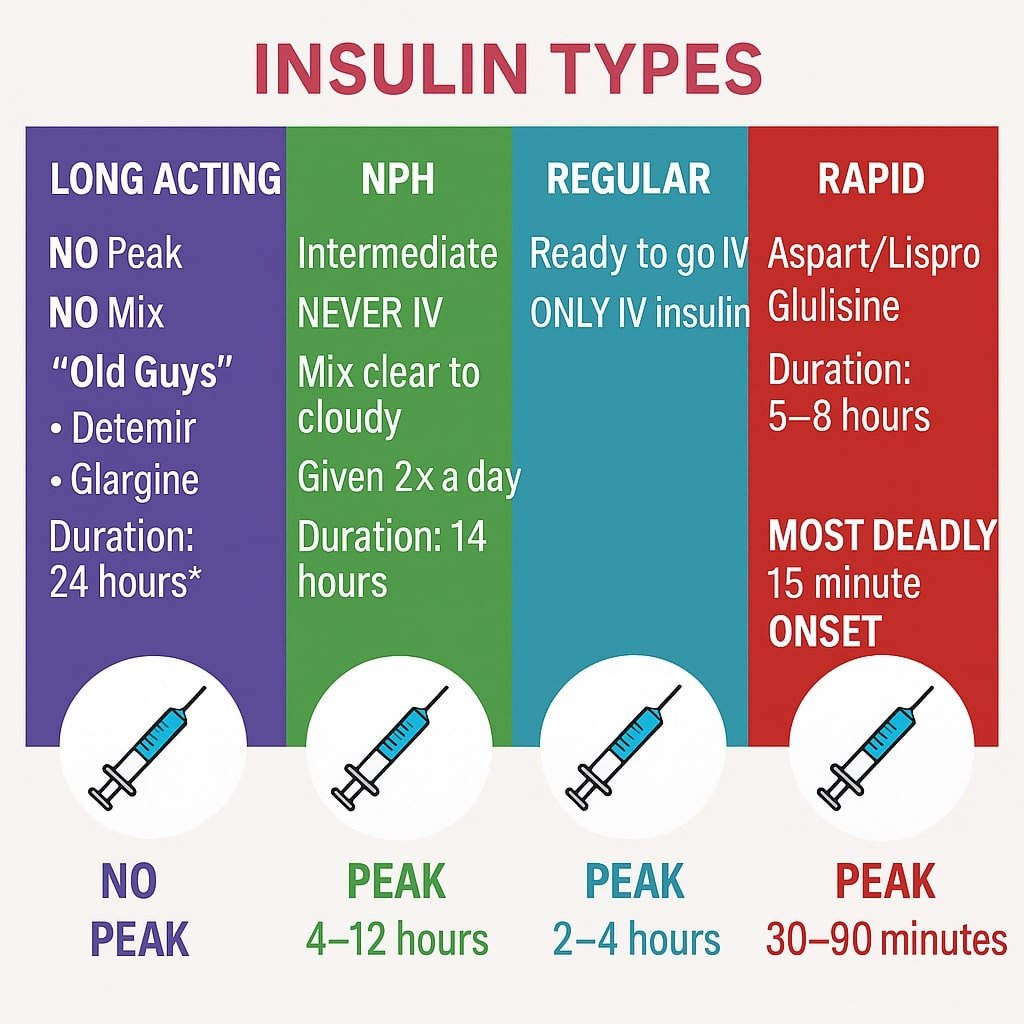
3.1 Rapid-Acting Insulin
- Examples: Insulin lispro, insulin aspart, insulin glulisine
- Onset: Usually within 10 to 15 minutes
- Peak: Approximately 1 to 2 hours
- Duration: Roughly 3 to 5 hours
- Usage Notes:
- Often taken just before or with meals to address post-meal spikes in blood glucose.
- Helps limit sharp increases in blood sugar after eating, but requires close monitoring to reduce the chance of low blood sugar when meals are postponed or smaller than anticipated.
3.2 Short-Acting (Regular) Insulin
- Examples: Humulin R, Novolin R
- Onset: Approximately 30 minutes
- Peak: Around 2 to 3 hours
- Duration: Can last up to 6 to 8 hours
- Usage Notes:
- Commonly injected 30 minutes before a meal to control glucose that rises after eating.
- Practical for hospital-based sliding scales, where dosing can be periodically adjusted based on glucose readings.
3.3 Intermediate-Acting Insulin (NPH)
- Examples: Humulin N, Novolin N
- Onset: Around 1 to 2 hours
- Peak: About 4 to 8 hours after injection
- Duration: May last 10 to 18 hours
- Usage Notes:
- Typically administered once or twice daily for background glucose management.
- Can be combined with rapid- or short-acting insulins to address mealtime surges as well as provide longer coverage.
3.4 Long-Acting Insulin
- Examples: Insulin glargine, insulin detemir
- Onset: 1 to 2 hours
- Peak: Minimal or “peakless” profile, meaning it remains steady
- Duration: Can last up to 24 hours, though individual responses vary
- Usage Notes:
- Usually taken once or twice per day to maintain consistent baseline levels.
- Aids in reducing overnight or fasting hyperglycemia when used as part of a coordinated approach to diabetes management.
3.5 Ultra-Long-Acting Insulin
- Example: Insulin degludec
- Onset: Approximately 1 hour
- Peak: Very flat profile with no pronounced peak
- Duration: Over 24 hours (some sources note duration up to 42 hours)
- Usage Notes:
- Reduces the number of daily injections needed in some treatment plans.
- Often applied in patients whose schedules or glucose patterns require a smoother, extended baseline coverage.
3.6 Combination (Pre-Mixed) Insulins
- Examples: 70/30, 50/50, or 75/25 mixes (vary by manufacturer)
- Components: A ratio of intermediate-acting insulin combined with either rapid-acting or short-acting insulin
- Onset, Peak, and Duration: Reflect the characteristics of both insulins included in the mixture
- Usage Notes:
- Simplifies dosing by offering coverage for both mealtime spikes and longer-term requirements in a single injection.
- Requires consistent meal and activity patterns since flexibility in adjusting meal-related doses separately can be limited.
Note: All times listed above are approximations and can differ based on individual response, injection site, and other factors. Adjustments to insulin regimens should be conducted under the guidance of a qualified healthcare provider.
4. Insulin Chart Basics
4.1 Explanation of Onset, Peak, and Duration
Every insulin type has characteristic phases:
- Onset: The estimated time before insulin starts to lower blood glucose.
- Peak: The period when insulin is most active.
- Duration: How long the insulin’s effect persists in the bloodstream.
By comparing these parameters for various insulins, healthcare providers and patients can select which formulation is most appropriate for specific times of the day. For example, short-acting insulin might be ideal before a meal to regulate immediate blood glucose rises, while a long-acting type may help maintain consistent levels over many hours.
4.2 Units of Measurement and Dosage Customization
- Insulin Units (IU): Most insulin vials and pens are labeled by International Units (IU).
- Personalized Dosing: Individuals often start on a general guideline prescribed by their physician, then adjust over time based on factors such as dietary choices, physical activity, and regular blood glucose readings.
- Self-Monitoring: Ongoing checks with a glucometer or continuous glucose monitor can signal when a dosage or timing change might be beneficial. Any modifications should typically be confirmed with a healthcare professional.
4.3 Standardized Insulin Charts (ADA Recommendations)
The American Diabetes Association (ADA) advocates for standardized reference materials that outline onset, peak, and duration ranges for each insulin type. These charts can:
- Help patients and clinicians visualize how specific insulins perform throughout the day.
- Serve as a practical guide in structuring injection schedules around meals, exercise, work, or school timetables.
- Reduce confusion by categorizing different insulin options under consistent metrics.
4.4 Importance of Time-Based Insulin Administration
- Meal Timing: Many insulin regimens work best when injections are carefully timed in relation to meals.
- Daily Routine: Injecting at consistent intervals helps keep blood sugar more predictable. Inconsistent schedules can result in unexpected low or high readings.
- Lifestyle Factors: Exercise, stress, sleep patterns, and shifts in routine may influence insulin demands. A well-structured chart accommodates these variables by aligning insulin doses with the patient’s typical activities.
Note:
While this overview covers core principles, insulin therapy must be tailored to individual needs. A qualified healthcare professional is best suited to guide dosage adjustments and refine strategies to achieve safer and more stable glucose levels.
5. Standard Insulin Charts
Thorough Review of USA-Approved Insulin Charts
Healthcare facilities in the United States rely on well-established insulin charts that have received professional recognition. Below are a few examples:
- Insulin Type vs. Action Time Chart
- Highlights the onset, peak, and duration for each category of insulin.
- Offers a general framework for planning mealtime and basal doses.
- Meal-Timed Insulin Chart
- Aligns insulin injection schedules with meals.
- Helps individuals structure meals to match insulin activity.
- Sliding Scale Insulin Chart
- Adjusts insulin doses based on current blood sugar levels.
- Aims to provide flexibility and address moment-to-moment changes.
- Basal-Bolus Insulin Schedule
- Divides total insulin doses into basal (background) and bolus (mealtime) injections.
- Often favored for achieving glucose levels that more closely resemble those of individuals without diabetes.
Visual Representation of Insulin Peaks and Durations
Many charts include graphs or tables to illustrate when insulin will be most active. Such visual aids help patients and providers decide the best times to inject insulin relative to meals and daily routines.
6. Personalizing an Insulin Chart
Gathering Relevant Patient Data
A tailored plan begins with understanding each individual’s:
- Blood Glucose Levels: Baseline readings and typical patterns.
- Carbohydrate Intake: How various meals affect glucose.
- Physical Activity Patterns: Frequency, intensity, and timing of exercise.
Collaborating with Healthcare Professionals
Medical teams, including endocrinologists, diabetes educators, and dietitians, play a critical role in helping individuals customize their insulin charts. Their expertise ensures that dosing strategies match each patient’s unique metabolic profile.
Tailoring Charts for Specific Needs
- Insulin Pump Users: Pump technology allows for more precise dose alterations based on ongoing blood sugar readings.
- Pregnant Patients: During pregnancy, insulin requirements and glucose targets may vary considerably, requiring close monitoring.
- Variable Work or Sleep Schedules: Shift workers or people with irregular sleep patterns may need specialized charts that accommodate frequent changes in daily routines.
7. Practical Use of Insulin Charts
7.1 Understanding the Purpose
Insulin charts serve as organized frameworks that outline when and how much insulin should be administered. By cross-referencing these charts with meal times, physical activity, and blood glucose levels, individuals and healthcare professionals can structure therapy to maintain more stable glucose control.
7.2 Matching Insulin Type with Daily Activities and Meals
- Timing: Short-acting or rapid-acting insulins are frequently administered before meals to address post-meal spikes, whereas long-acting options are intended to maintain a baseline throughout the day.
- Meal Planning: Meal-based charts specify precise injection times so that insulin action aligns with carbohydrate intake. This approach can lower the likelihood of unexpected highs or lows.
- Physical Activity: Those who exercise regularly can adjust their chart to ensure that insulin doses do not coincide with intense activity, minimizing risks of low blood glucose.
7.3 Adjusting Dosages Based on Blood Sugar Trends
- Pattern Recognition: Tracking consistent high or low readings at specific times can indicate a need to alter insulin amounts or injection times.
- Daily Logs: Logging blood glucose levels before and after meals, as well as any relevant symptoms, helps identify when adjustments might be needed.
- Healthcare Collaboration: Major dose changes should be verified with medical professionals, who can suggest incremental or more significant modifications based on logs and clinical standards.
7.4 Incorporating Carbohydrate Counting
- Meal-Based Dosing: Charts often integrate carbohydrate ratios that inform how much rapid-acting insulin is given for a set amount of carbohydrates.
- Immediate Feedback: When carbohydrate counting is combined with an insulin chart, patients can adjust doses in real time, guided by the chart’s recommended range for mealtime bolus injections.
7.5 Documenting Patterns and Anomalies
- Record Keeping: Noting unusual circumstances (e.g., illness, stress, or dietary changes) next to insulin doses helps explain unexpected glucose fluctuations.
- Trend Analysis: Reviewing records weekly or monthly can reveal recurring themes, such as consistently higher readings at the same time of day.
7.6 Integration with Monitoring Devices
- Continuous Glucose Monitors (CGMs): Users can synchronize CGM readings with their insulin chart, allowing quicker responses to fluctuating glucose levels.
- Insulin Pumps: Some devices automate dosage changes according to CGM data. Maintaining an up-to-date chart ensures that these automated suggestions align with established therapeutic goals.
7.7 Collaboration with Healthcare Providers
- Professional Input: Physicians, diabetes educators, and dietitians can validate whether charts reflect best practices and the patient’s evolving health status.
- Routine Evaluations: Regular check-ins allow for timely updates to the chart. This is particularly important when faced with changes in weight, activity level, or other health indicators.
7.8 Handling Special Situations
- Missed Doses: Marking missed or late doses on the chart helps identify potential causes of erratic glucose readings. It also highlights areas for improvement in daily routines.
- Illness or Stress: Both can significantly impact insulin sensitivity. Adjusting doses during periods of illness, guided by medical advice, can prevent serious deviations in glucose levels.
- Travel: Shifts in time zones and meal patterns require careful adjustments to maintain consistent dosing intervals.
7.9 Combining Paper and Digital Tools
- Paper Logs: Convenient for everyday note-taking and visual reminders. They do not require technical knowledge or electronic devices.
- Digital Platforms: Offer automated data analysis, graphing capabilities, and the option to share records with healthcare providers in real time. Some individuals prefer a hybrid model of using both paper and digital methods to capture all relevant details.
Note: The strategies outlined above should be adapted to individual circumstances. Always consult a qualified healthcare professional for personalized insulin therapy and charting guidelines.
8. Insulin Chart Formats
8.1 Paper-Based Templates
- Daily Logs
- These templates outline hour-by-hour insulin doses, meal times, and blood glucose readings for a single day.
- They are straightforward to use, particularly for individuals who prefer or require physical records.
- Weekly Planners
- Provide an overview of recurring events, meal schedules, or work shifts.
- Display potential patterns in insulin requirements over multiple days, assisting with more accurate adjustments.
- Monthly Overviews
- Offer a long-term perspective on how changes in diet, physical activity, or medications affect glucose levels.
- Allow healthcare professionals to monitor trends such as recurring hyperglycemia or hypoglycemia at specific periods.
8.2 Spreadsheet Tools
- Customizable Layouts
- Software applications like Microsoft Excel or Google Sheets provide templates for logging insulin dosages and glucose measurements.
- Users can add automated formulas to highlight out-of-range values or average their readings over time.
- Data Collaboration
- Spreadsheet files can be shared with healthcare teams, making remote consultations more efficient.
- The ability to store and access files online supports data continuity across multiple devices.
8.3 Mobile Applications
- Integrated Features
- Many apps link to glucose meters, pulling real-time blood sugar data directly into logs.
- Push notifications remind users when it is time to check glucose or administer insulin, helping reduce missed doses.
- Graphical Analysis
- Apps often include charts or color-coded indicators to illustrate trends or patterns, making it simpler to evaluate effectiveness.
- Some applications generate summary reports that can be emailed or shared at medical appointments.
- Accessibility and Convenience
- A quick setup process and user-friendly designs make these tools accessible to a wide range of age groups and technological skill levels.
- Many apps feature secure cloud backup solutions, adding an extra layer of data protection.
8.4 Wearable and Connected Devices
- Continuous Glucose Monitors (CGMs)
- CGMs measure blood sugar at regular intervals throughout the day, providing near real-time feedback.
- When linked to compatible insulin pumps, they can automatically recommend adjustments based on current readings.
- Smartwatches and Activity Trackers
- Users can view notifications or real-time glucose data on their wrist, facilitating quicker responses to unexpected glucose changes.
- Built-in fitness tracking features capture steps taken or calories burned, helping correlate insulin needs with daily activities.
8.5 Hybrid Approaches
- Combination of Paper and Digital
- Some individuals may prefer writing daily notes on paper and later digitizing the data for comprehensive analysis.
- This hybrid system provides the ease of handwritten annotations with the convenience of long-term data storage.
- Collaborative Platforms
- Some electronic health record (EHR) systems integrate with personal health apps, enabling direct uploads of insulin data.
- Consolidating information into one accessible location streamlines communication among multiple healthcare providers.
Note: Selecting the right insulin chart format may depend on factors such as personal preferences, technology access, and medical circumstances. Working with a healthcare team to establish a sustainable recording process can enhance both short- and long-term diabetes management.
9. Troubleshooting and Adjustments
Common Challenges in Insulin Management
- Missed Doses: Failing to administer an insulin dose on time can quickly shift blood sugar levels outside the normal range.
- Overdosing or Underdosing: Taking too much or too little insulin can cause severe fluctuations in glucose.
- Variability in Blood Glucose Levels: Even small changes in routine can influence insulin requirements.
Recognizing Patterns of Hyperglycemia and Hypoglycemia
- Hyperglycemia: Persistent high blood sugar, often accompanied by increased thirst and frequent urination.
- Hypoglycemia: Low blood sugar, causing symptoms like shaking, sweating, or confusion.
Identifying trends in these events can suggest that adjustments to insulin charts are necessary.
Factors Affecting Insulin Requirements
- Stress and Illness: The body’s stress response can modify glucose handling, necessitating different insulin doses.
- Physical Activity and Lifestyle Changes: Exercise frequency, diet alterations, or lifestyle variations all influence blood sugar control.
10. USA Health Guidelines on Insulin Use
Overview of Key Organizations and Their Roles
- American Diabetes Association (ADA):
- Publishes position statements and guidelines on the selection and timing of insulin therapies.
- Encourages individualized regimens that account for a patient’s daily routines, meal schedules, and glucose targets.
- Centers for Disease Control and Prevention (CDC):
- Addresses public health aspects of diabetes, including preventive measures and ongoing management strategies.
- Provides resources on safe handling of insulin, needle disposal, and monitoring outcomes.
- Food and Drug Administration (FDA):
- Oversees the approval and labeling of insulin products in the United States.
- Specifies manufacturing standards, purity levels, and expiration requirements for all insulin formulations.
Best Practices for Safe Use of Insulin
- Adherence to Prescribed Dosages and Schedules
- Following the dose and timing specified by a healthcare provider is critical for stable blood glucose control.
- Any modifications—especially changes in meal patterns or activity levels—should be reviewed with a medical professional.
- Storage and Temperature Control
- Store unused insulin in a refrigerator (generally between 36°F and 46°F).
- Once in use or not refrigerated, keep insulin away from direct heat or freezing conditions, following manufacturer guidelines.
- Proper Injection Techniques
- Seek instruction on injection sites (e.g., abdomen, thigh, or upper arm) and rotate these sites to reduce tissue complications.
- Dispose of needles and syringes in approved sharps containers in accordance with local regulations.
- Monitoring Blood Glucose Levels
- Frequent testing helps track responses to insulin and identifies early signs of hyperglycemia or hypoglycemia.
- Recording blood glucose readings in a log or digital app supports discussions with healthcare professionals during appointments.
- Handling Missed or Delayed Doses
- Missing or postponing an insulin dose can lead to blood sugar fluctuations.
- Individuals should note missed doses in their log and contact a healthcare provider if multiple incidents occur.
Monitoring Outcomes and Preventive Care
- Regular Medical Check-Ups
- Scheduled appointments allow physicians or diabetes specialists to review medication effectiveness, A1C levels, and general health markers.
- Adjustments to insulin regimens may be made based on trends observed in lab results or personal monitoring records.
- Routine Screenings
- Periodic evaluations of heart health, kidney function, and eye health can detect complications early.
- Foot exams also play a role in identifying circulation or nerve problems related to diabetes.
- Continuing Education and Support
- Diabetes education programs, offered by many clinics, teach practical skills for reading labels, meal planning, and managing stress.
- Online support groups and telemedicine consultations can enhance day-to-day management guidance.
Reporting Adverse Effects and Concerns
- Hypoglycemia or Hyperglycemia Episodes: Seek medical advice if experiencing recurring episodes of low or high blood glucose.
- Allergic Reactions or Injection Site Issues: Reactions like redness, swelling, or intense itching require prompt evaluation.
- Access to Emergency Services: Individuals should know when to contact emergency services, such as in cases of severe low blood sugar or diabetic ketoacidosis.
Importance of a Comprehensive Approach
USA health guidelines emphasize the value of consistent collaboration between patients and healthcare teams. In addition to adhering to dosing schedules, other lifestyle factors—such as balanced nutrition, regular physical activity, and stress management—contribute to stable blood glucose. Individuals are encouraged to keep open lines of communication with healthcare providers to address any shifts in insulin requirements or overall health status.
Disclaimer:
The information presented here is intended as a general guide. Always follow the advice of qualified healthcare professionals regarding insulin therapy and any related health decisions.
11. Frequently Used Insulin Charts
1. What is an insulin chart, and why do I need one?
An insulin chart is a structured guideline for tracking insulin dosages, timing, and blood glucose levels. It helps individuals with diabetes maintain consistent, accurate management of their condition. By referencing a chart, you and your healthcare provider can more effectively identify trends and make timely dosage adjustments.
2. Which insulin chart is best for beginners?
A sliding scale chart is often recommended for those new to insulin therapy. It bases insulin doses on current blood glucose readings and offers straightforward adjustments. However, always consult your healthcare professional before selecting a specific method.
3. How do I know if I should use a basal-bolus chart versus a fixed-dose chart?
The choice depends on your diabetes type, lifestyle, and treatment goals. Basal-bolus charts typically suit individuals requiring tight glucose control and flexibility. Fixed-dose charts are more rigid but can be simpler to follow. A healthcare provider can recommend the best approach for your situation.
4. Do insulin charts differ between Type 1 and Type 2 diabetes?
While the fundamental principles remain the same, Type 1 patients often rely more heavily on daily insulin and detailed scheduling. Type 2 patients may employ insulin charts in combination with oral medications and lifestyle interventions. The exact chart format may vary based on individual needs.
5. Are there different charts for gestational diabetes?
Yes. Pregnancy brings unique insulin demands, and charts for gestational diabetes usually feature more frequent monitoring and smaller, carefully adjusted doses. Obstetricians and endocrinologists commonly collaborate to develop these specialized charts.
6. How often should I update my insulin chart?
It is advisable to review and update your chart whenever there is a significant change in your routine, such as a shift in diet, exercise habits, or work schedule. Additionally, periodic check-ups with a healthcare professional will help ensure your insulin chart remains accurate.
7. Can I use an app or digital tool to replace a traditional paper-based insulin chart?
Absolutely. Many reputable apps integrate with glucose monitors and insulin pumps, allowing for real-time updates and reminders. While digital solutions offer convenience, it is essential to use platforms that follow HIPAA guidelines or other privacy regulations to protect your health data.
8. How do I handle missed doses or unexpected blood sugar readings?
When you miss a dose or encounter unexpectedly high or low glucose levels, record the incident in your chart. This record helps in assessing trends and prevents repeated oversights. Always consult a medical professional to determine the safest corrective measures.
12. Real-Life Case Studies
Case Study 1: Structured Insulin Chart for Type 1 Diabetes
Profile
- Patient: A 25-year-old university student
- Medical Background: Diagnosed with Type 1 diabetes at age 12
- Primary Challenge: Balancing academic schedule and meal timings
Approach
- Basal-Bolus Routine: The patient relies on a long-acting (basal) insulin administered once daily, supplemented with rapid-acting (bolus) insulin before each meal.
- Insulin Chart: Displays time of dose, carbohydrate content of meals, and corresponding blood glucose readings throughout the day.
- Key Observations: Frequent nighttime hypoglycemia initially required a small reduction in the evening basal dose.
- Outcome: By aligning the chart with class schedules, meal plans, and glucose checks, the patient achieved more consistent blood glucose readings and reduced the likelihood of overnight low blood sugar.
Case Study 2: Managing Gestational Diabetes with Sliding Scale Insulin
Profile
- Patient: A 32-year-old pregnant individual in the third trimester
- Medical Background: Gestational diabetes identified during routine prenatal screenings
- Primary Challenge: Fluctuating blood glucose levels due to hormonal changes
Approach
- Sliding Scale Chart: Enables dose adjustments based on pre-meal and post-meal blood glucose.
- Close Monitoring: Obstetrician and endocrinologist review weekly logs to account for hormonal variations and fetal growth requirements.
- Additional Considerations: Emphasis placed on meal spacing and moderate exercise tailored to each trimester.
- Outcome: Through frequent blood glucose checks and ongoing data review, the patient maintained stable glucose control, reducing risks associated with high or low blood sugar during pregnancy.
Case Study 3: Adjusting Insulin for High-Intensity Physical Activity
Profile
- Patient: A 40-year-old recreational athlete diagnosed with Type 2 diabetes
- Medical Background: Regular high-intensity workouts and a family history of diabetes
- Primary Challenge: Preventing post-exercise hypoglycemia while managing overall blood glucose
Approach
- Integrated Chart: Combines daily basal doses with flexible bolus injections timed around exercise sessions.
- Frequent Monitoring: Uses a continuous glucose monitor to check levels before, during, and after workouts.
- Nutritional Adjustments: Considers pre-workout snacks to offset potential dips in blood sugar caused by extended or intense exercise.
- Outcome: The patient effectively minimized hypoglycemia and improved overall glucose stability through individualized modifications tracked on the insulin chart.
Important Note: The scenarios described above are illustrative examples. Actual treatment plans vary, and any changes to insulin regimens should only be made under the guidance of qualified healthcare professionals.
13. Tools and Resources
- Mobile Apps for Insulin and Blood Sugar Management
- Offer timely reminders, trend graphs, and integration with wearables.
- Trusted Healthcare Websites (ADA, CDC, NIH)
- Provide patient-friendly materials, including printable charts and step-by-step management guides.
- Printable Insulin Chart Templates
- Can be found through professional organizations or health portals.
- Enable convenient logging of insulin doses, blood sugar levels, and meal details.
- Support Groups and Online Forums
- Offer community-driven insights and shared experiences.
- A place to ask questions or discuss challenges related to insulin use.
14. Conclusion
It is clear that insulin charts are a cornerstone of diabetes care, helping individuals plan and monitor therapy. By coordinating with healthcare professionals and adopting standardized charts that meet ADA and CDC standards, individuals can achieve more consistent blood sugar levels and a better quality of life. Regular reviews and updates of these charts—especially when underlying health or lifestyle factors shift—are equally important to stay aligned with best practices.
Thought about reference generation for health articles for 15 seconds
Below is a concise set of example references that follow standard citation practices and align with authoritative health sources, including Google Health. When using them in an article, ensure each reference is formatted according to your chosen style (e.g., APA, MLA).
References
- Google Health. (n.d.). Diabetes and Insulin: Key Facts and Management Guidelines. Retrieved [Month Day, Year], from https://health.google.com/diabetes-insulin-management
- American Diabetes Association. (2023). Standards of Medical Care in Diabetes—2023. Diabetes Care, 46(Supplement 1), S1–S314.
- Centers for Disease Control and Prevention. (2022). Insulin Basics. Retrieved [Month Day, Year], from https://www.cdc.gov/diabetes/managing/insulin.html
- National Institutes of Health. (2021). Insulin, Medicines, & Other Diabetes Treatments. Retrieved [Month Day, Year], from https://www.niddk.nih.gov/health-information/diabetes/overview/insulin-medicines-treatments
- Mayo Clinic. (2022). Diabetes Treatment: Insulin Therapy for Diabetes. Retrieved [Month Day, Year], from https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetes-treatment/art-20044084