1. Introduction
1.1 Overview of Insulin Autoimmune Syndrome (IAS)
Insulin Autoimmune Syndrome (IAS), also known as Hirata’s disease, is a rare condition characterized by the body’s immune system mistakenly producing antibodies against insulin. These autoantibodies interfere with insulin’s normal function, leading to unpredictable fluctuations in blood glucose levels. Initially, individuals with IAS may experience episodes of hypoglycemia (abnormally low blood sugar levels) due to the excessive binding of insulin by these antibodies, which subsequently release insulin unpredictably, causing hyperglycemia (elevated blood sugar levels). This erratic behavior results in challenging management of blood glucose, posing significant risks if left untreated.
IAS primarily affects individuals without a prior history of diabetes, distinguishing it from other insulin-related disorders. The syndrome is often associated with the consumption of certain medications, particularly those containing sulfhydryl groups, which are believed to trigger the autoimmune response. Understanding the mechanisms and triggers of IAS is crucial for timely diagnosis and effective management, thereby preventing potential complications related to unstable blood glucose levels.
1.2 Historical Background
The first identification of Insulin Autoimmune Syndrome dates back to Japan in 1970 when Dr. Hirata and his colleagues reported cases involving patients who developed insulin autoantibodies without prior insulin therapy. This groundbreaking discovery challenged the existing understanding of insulin-related disorders, highlighting the possibility of autoimmune mechanisms in insulin regulation.
Over the subsequent decades, research into IAS expanded, uncovering its association with specific medications, particularly those used to treat hypertension and hyperlipidemia, such as methimazole and certain alpha-lipoic acid supplements. The prevalence of IAS has been observed to vary geographically, with higher incidence rates reported in East Asian populations compared to Western countries. This disparity suggests potential genetic predispositions that influence the susceptibility to IAS.
Advancements in immunological assays and diagnostic techniques have facilitated more accurate detection of insulin autoantibodies, enabling better characterization of the syndrome. Despite being a recognized medical condition for over fifty years, IAS remains relatively uncommon, and ongoing research continues to explore its underlying mechanisms, risk factors, and optimal management strategies.
1.3 Importance of Understanding IAS
Comprehending Insulin Autoimmune Syndrome is essential for several reasons, particularly due to its implications for patient health and the broader understanding of autoimmune disorders. Firstly, IAS presents with symptoms that can mimic other more common conditions, such as type 1 or type 2 diabetes, making accurate diagnosis challenging. Misdiagnosis can lead to inappropriate treatment strategies, potentially exacerbating the patient’s condition.
Secondly, IAS underscores the intricate relationship between the immune system and metabolic regulation. By studying IAS, medical professionals can gain deeper insights into how autoantibodies affect hormone function and glucose metabolism, which may have broader applications in understanding and treating other autoimmune and endocrine disorders.
Furthermore, recognizing the triggers and risk factors associated with IAS, such as specific medications, is crucial for prevention and management. Healthcare providers can make informed decisions regarding the prescription of drugs known to be associated with IAS, especially in populations at higher risk. Additionally, early identification of IAS allows for timely interventions to stabilize blood glucose levels, thereby reducing the risk of acute complications like seizures, loss of consciousness, or even death due to severe hypoglycemia.
2. Understanding Insulin Autoimmune Syndrome
2.1 Definition and Classification
Insulin Autoimmune Syndrome (IAS) is a rare endocrine disorder characterized by the presence of autoantibodies directed against endogenous insulin. Unlike typical forms of diabetes, IAS occurs in individuals who have not previously been exposed to exogenous insulin therapy. The condition leads to abnormal regulation of insulin, resulting in fluctuating blood glucose levels that can oscillate between hypoglycemia and hyperglycemia.
IAS is classified as one of the insulin receptoropathies, a group of disorders involving the malfunction of insulin receptors or insulin itself. Within this category, IAS is distinct due to its autoimmune nature, where the body’s immune system mistakenly targets insulin molecules. This classification is crucial for differentiating IAS from other insulin-related disorders such as insulinoma (a tumor producing excess insulin) and type 1 diabetes mellitus, where autoimmunity targets insulin-producing beta cells in the pancreas rather than insulin molecules directly.
The classification of IAS can further be subdivided based on the underlying triggers and associated factors. Primary IAS occurs without any identifiable external factors, whereas secondary IAS is linked to specific precipitating elements such as certain medications, infections, or genetic predispositions. This distinction aids in understanding the etiology of the syndrome and tailoring appropriate management strategies for affected individuals.
2.2 Epidemiology and Prevalence
Insulin Autoimmune Syndrome is an uncommon condition with varying prevalence across different populations. Epidemiological studies indicate a higher incidence in East Asian countries, particularly Japan, where the majority of documented cases originate. In contrast, reports from Western nations remain scarce, suggesting possible genetic or environmental factors that influence susceptibility.
The prevalence of IAS is estimated to be less than 1% among individuals presenting with hypoglycemic episodes. However, the exact incidence is challenging to determine due to underdiagnosis and misclassification, as IAS can mimic other more prevalent conditions like type 1 diabetes or insulinoma. Increased awareness and improved diagnostic techniques have contributed to a gradual rise in reported cases, but IAS remains a relatively rare diagnosis in the global context.
Demographic factors such as age and gender also play a role in the epidemiology of IAS. The syndrome predominantly affects adults, with a slight female predominance observed in several studies. Additionally, certain genetic markers, particularly specific HLA (human leukocyte antigen) alleles, have been associated with a higher risk of developing IAS, especially in East Asian populations. These genetic predispositions highlight the interplay between heredity and environmental triggers in the manifestation of the syndrome.
Understanding the epidemiological landscape of IAS is essential for healthcare providers to recognize potential cases, especially in regions with higher prevalence. It also underscores the importance of considering IAS in differential diagnoses when patients present with unexplained hypoglycemia, thereby facilitating timely and accurate identification of the condition.
2.3 Pathophysiology of IAS
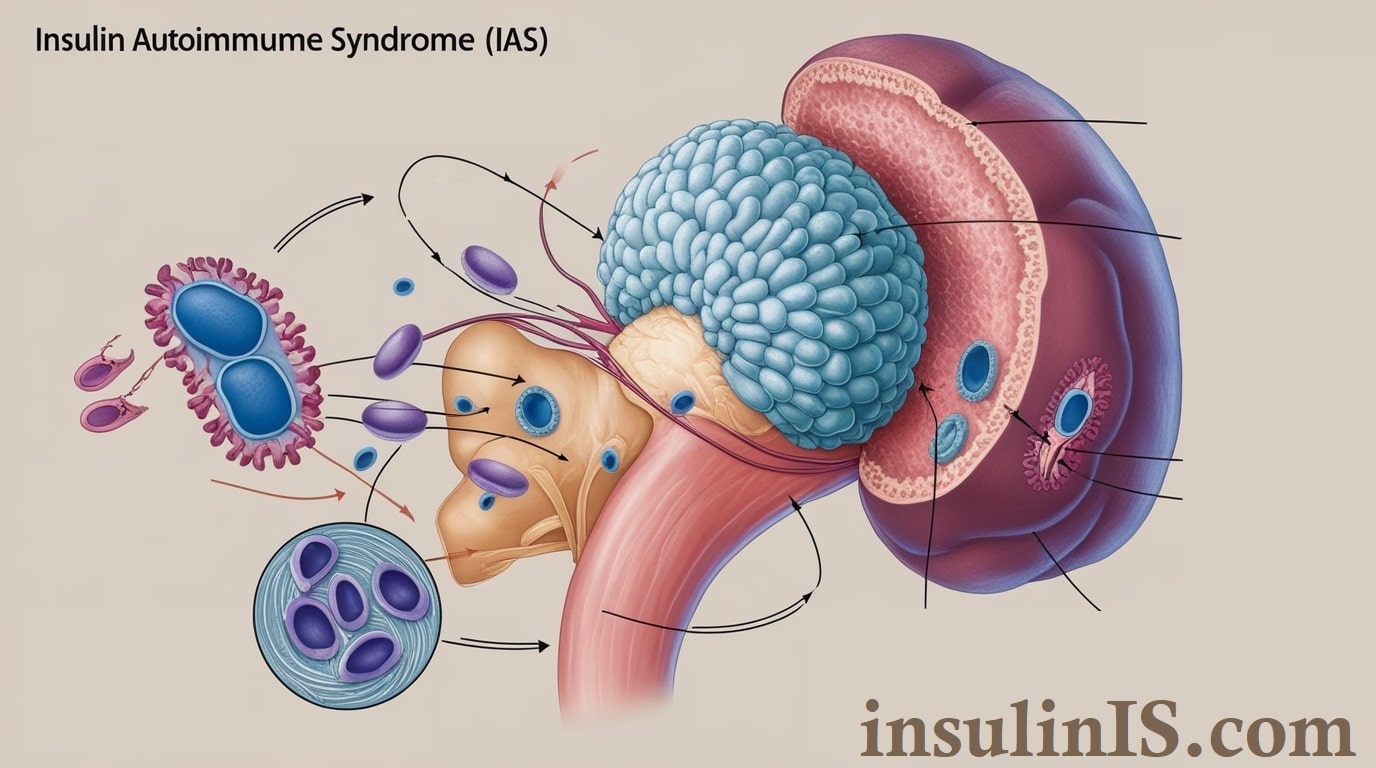
The pathophysiological mechanisms underlying Insulin Autoimmune Syndrome involve a complex interplay between the immune system and insulin regulation. Central to IAS is the production of autoantibodies that specifically target endogenous insulin molecules. These autoantibodies bind to insulin, forming insulin-antibody complexes that disrupt the normal bioavailability and activity of insulin.
Under typical circumstances, insulin facilitates the uptake of glucose by cells, thereby maintaining blood glucose homeostasis. In IAS, the binding of autoantibodies to insulin impairs this process in two primary ways. Initially, the autoantibodies sequester insulin, reducing its free concentration and leading to periods of insulin deficiency and resultant hyperglycemia. Subsequently, these complexes can release insulin unpredictably, causing transient surges in insulin levels and subsequent hypoglycemia.
The fluctuation between insulin binding and release creates a state of glycemic instability, where patients experience alternating episodes of low and high blood sugar levels. This erratic insulin activity is further compounded by the body’s attempt to compensate for the impaired insulin function, leading to a vicious cycle of metabolic dysregulation.
Genetic factors play a significant role in the susceptibility to IAS. Certain HLA alleles, particularly HLA-DR4 and HLA-DRB1*04:06, have been strongly associated with the development of insulin autoantibodies. These genetic markers influence the immune system’s propensity to recognize insulin as a foreign antigen, thereby facilitating the autoimmune response.
Environmental triggers, such as the ingestion of sulfhydryl-containing medications, are also implicated in the pathogenesis of IAS. These substances may alter insulin molecules or influence immune cell activity, promoting the formation of autoantibodies. Additionally, oxidative stress and molecular mimicry, where foreign antigens resemble endogenous insulin, can further exacerbate the autoimmune response.
3. Causes and Risk Factors
Understanding the underlying causes and risk factors of Insulin Autoimmune Syndrome (IAS) is essential for identifying individuals at risk, implementing preventive measures, and developing effective treatment strategies. This section delves into the various genetic, environmental, and medication-related factors that contribute to the onset of IAS, as well as other significant contributors.
3.1 Genetic Factors
Genetic predisposition plays a pivotal role in the susceptibility to Insulin Autoimmune Syndrome. Certain genetic markers, particularly specific human leukocyte antigen (HLA) alleles, have been strongly associated with an increased risk of developing IAS. Notably, the HLA-DR4 and HLA-DRB1*04:06 alleles are frequently identified in individuals diagnosed with IAS, especially within East Asian populations. These alleles are involved in the regulation of the immune system, influencing how the body recognizes and responds to insulin molecules.
The presence of these HLA alleles facilitates the presentation of insulin peptides to immune cells, potentially triggering an autoimmune response against endogenous insulin. This genetic linkage underscores the importance of heredity in the pathogenesis of IAS and suggests that individuals carrying these alleles may have a heightened vulnerability to developing the syndrome when exposed to other risk factors.
Furthermore, family studies indicate that IAS can occur more frequently among relatives, reinforcing the concept of a hereditary component. However, it is important to note that possessing these genetic markers does not guarantee the development of IAS; rather, it signifies an increased predisposition that may be influenced by additional factors.
3.2 Environmental Triggers
Environmental factors are significant contributors to the manifestation of Insulin Autoimmune Syndrome. Various external elements can interact with an individual’s genetic makeup to initiate or exacerbate the autoimmune response against insulin. Key environmental triggers include:
- Infections: Certain viral or bacterial infections may act as catalysts for the immune system to erroneously target insulin. The molecular mimicry phenomenon, where infectious agents possess antigens resembling insulin, can confuse the immune system, leading to the production of autoantibodies.
- Dietary Components: The consumption of specific foods or supplements containing sulfhydryl groups has been linked to the onset of IAS. These compounds can modify insulin molecules, making them more immunogenic and prone to being targeted by the immune system.
- Lifestyle Factors: Stress, exposure to toxins, and other lifestyle-related factors can influence immune system function. Chronic stress, for instance, may disrupt immune regulation, increasing the likelihood of autoimmune reactions.
- Geographical Variations: The prevalence of IAS in certain regions, particularly East Asia, suggests that regional environmental factors, such as prevalent dietary habits or exposure to specific environmental agents, may contribute to the syndrome’s development.
3.3 Medication-Induced IAS
Medication-induced Insulin Autoimmune Syndrome is a well-documented phenomenon wherein certain pharmaceutical agents trigger the autoimmune response against insulin. Medications containing sulfhydryl groups are particularly implicated in this process. These drugs can alter the structure of insulin or its binding proteins, rendering insulin molecules more recognizable to the immune system as foreign entities. Common medications associated with IAS include:
- Methimazole: An antithyroid medication used to treat hyperthyroidism, methimazole has been frequently linked to the development of insulin autoantibodies, leading to IAS.
- Alpha-Lipoic Acid Supplements: Often used as a dietary supplement for its antioxidant properties, alpha-lipoic acid can modify insulin molecules, increasing the risk of an autoimmune response.
- Other Sulfhydryl-Containing Drugs: Various other medications used to treat conditions such as hypertension, rheumatoid arthritis, and epilepsy contain sulfhydryl groups and have been associated with IAS in some cases.
The temporal relationship between the initiation of these medications and the onset of IAS symptoms is a critical factor in establishing causality. Clinicians are advised to monitor patients starting on these medications for any signs of hypoglycemia or other related symptoms indicative of IAS.
3.4 Other Contributing Factors
In addition to genetic, environmental, and medication-related factors, several other elements may contribute to the development of Insulin Autoimmune Syndrome:
- Underlying Health Conditions: Individuals with pre-existing autoimmune disorders, such as rheumatoid arthritis or systemic lupus erythematosus, may have an increased risk of developing IAS due to the already heightened state of immune dysregulation.
- Age and Gender: IAS can occur at any age but is more commonly diagnosed in middle-aged and older adults. Additionally, a slight female predominance has been observed in several studies, suggesting that hormonal or sex-related factors may influence susceptibility.
- Metabolic Stress: Conditions that impose metabolic stress, such as severe infections, surgery, or trauma, can disrupt normal insulin regulation and immune function, potentially triggering IAS in susceptible individuals.
- Nutritional Deficiencies: Deficiencies in certain nutrients that are vital for immune system regulation, such as vitamin D or selenium, may impair immune tolerance mechanisms, increasing the likelihood of autoimmune responses.
- Hormonal Influences: Fluctuations in hormone levels, particularly those related to the endocrine system, may impact immune system behavior and insulin metabolism, contributing to the onset of IAS.
4. Clinical Presentation
Insulin Autoimmune Syndrome (IAS) manifests through a variety of clinical symptoms that result from the dysregulation of insulin activity. Understanding the clinical presentation of IAS is crucial for timely diagnosis and effective management. This section explores the common symptoms experienced by individuals with IAS, distinguishes between acute and chronic manifestations, and examines the syndrome’s impact on daily life.
4.1 Common Symptoms
The clinical symptoms of Insulin Autoimmune Syndrome primarily stem from the erratic behavior of insulin due to the presence of autoantibodies. These symptoms are largely related to abnormal blood glucose levels and can vary in severity and frequency. Common symptoms include:
- Hypoglycemia: Episodes of low blood sugar are the most prevalent symptom. Individuals may experience sudden weakness, shakiness, sweating, confusion, and dizziness. Severe hypoglycemia can lead to loss of consciousness, seizures, or even coma if not promptly addressed.
- Hyperglycemia: Paradoxically, IAS can also cause periods of high blood sugar. Symptoms may include increased thirst, frequent urination, fatigue, and blurred vision. These fluctuations between low and high blood sugar levels can create a challenging clinical scenario.
- Neuroglycopenic Symptoms: Due to insufficient glucose supply to the brain during hypoglycemic episodes, individuals may experience headaches, difficulty concentrating, mood disturbances, and impaired cognitive function.
- Autonomic Symptoms: The autonomic nervous system may be affected, leading to palpitations, anxiety, and hunger pangs during hypoglycemic episodes.
- Gastrointestinal Symptoms: Some patients report nausea, vomiting, and abdominal discomfort, which can be attributed to both hypoglycemia and the underlying autoimmune process.
4.2 Acute vs. Chronic Manifestations
The manifestations of IAS can be categorized based on their temporal nature—acute or chronic—and understanding this distinction aids in appropriate clinical management.
Acute Manifestations
Acute presentations of IAS are characterized by sudden and severe episodes of hypoglycemia. These episodes can occur without warning and may be triggered by factors such as fasting, exercise, or stress. Acute symptoms necessitate immediate medical attention to prevent complications. Key features include:
- Sudden Onset: Rapid development of hypoglycemic symptoms without prior indication.
- Severe Hypoglycemia: Profound drops in blood sugar levels that can lead to loss of consciousness or seizures.
- Emergency Situations: Acute episodes may require urgent intervention, including glucose administration or intravenous dextrose, to stabilize the patient.
Chronic Manifestations
Chronic manifestations involve ongoing fluctuations in blood glucose levels, leading to persistent and recurrent symptoms over an extended period. These manifestations can significantly impact an individual’s quality of life and may include:
- Frequent Hypoglycemic Episodes: Repeated low blood sugar events that disrupt daily activities and sleep patterns.
- Intermittent Hyperglycemia: Periods of elevated blood sugar that may contribute to long-term complications if not managed effectively.
- Chronic Fatigue: Persistent tiredness and lack of energy resulting from unstable glucose levels.
- Cognitive Impairment: Long-term effects on memory, concentration, and overall cognitive function due to recurrent neuroglycopenia.
- Emotional and Psychological Impact: Ongoing stress, anxiety, and mood swings associated with the unpredictability of blood glucose fluctuations.
4.3 Impact on Daily Life
The unpredictable nature of Insulin Autoimmune Syndrome can have profound effects on various aspects of an individual’s daily life. The constant management of fluctuating blood glucose levels poses significant challenges, influencing both physical and psychological well-being.
- Lifestyle Adjustments: Individuals with IAS often need to make significant changes to their diet and meal schedules to manage blood sugar levels. This may include frequent monitoring of blood glucose, adhering to strict meal plans, and avoiding activities that could precipitate hypoglycemia.
- Occupational Challenges: Maintaining consistent blood glucose levels is essential for optimal cognitive and physical performance. Fluctuations can impair work efficiency, increase the risk of accidents, and necessitate accommodations in the workplace.
- Social Activities: Participation in social events involving food can become stressful due to the need to manage insulin levels carefully. Individuals may feel restricted or anxious about potential hypoglycemic episodes in public settings.
- Emotional Well-Being: The unpredictability of IAS can lead to chronic stress, anxiety, and a diminished sense of control over one’s health. The fear of sudden hypoglycemia can affect personal relationships and overall mental health.
- Healthcare Dependence: Continuous medical supervision and frequent consultations with healthcare providers are often required to manage IAS effectively. This ongoing need for medical attention can be burdensome and impact an individual’s independence.
- Quality of Life: The cumulative effect of managing IAS can lead to a reduced quality of life, affecting physical health, emotional stability, and social interactions. Support systems, including family, friends, and healthcare professionals, play a crucial role in mitigating these impacts.
5. Diagnosis of Insulin Autoimmune Syndrome
Accurate diagnosis of Insulin Autoimmune Syndrome (IAS) is critical for effective management and prevention of complications. Diagnosing IAS involves a combination of clinical evaluation, laboratory testing, differential diagnosis, and adherence to established diagnostic criteria. This section outlines the comprehensive approach required to identify IAS, ensuring that healthcare providers can distinguish it from other similar conditions and implement appropriate treatment strategies.
5.1 Clinical Assessment
The initial phase of diagnosing IAS involves a detailed clinical assessment aimed at identifying symptoms and understanding the patient’s medical history. Key components of the clinical assessment include:
- Symptom Evaluation: Patients with IAS typically present with episodes of hypoglycemia, which may manifest as dizziness, sweating, confusion, palpitations, or even loss of consciousness. It is essential to document the frequency, duration, and triggers of these episodes to understand the pattern and severity of the syndrome.
- Medical History: A thorough medical history helps in identifying potential risk factors and underlying conditions. This includes investigating any recent changes in medication, particularly the use of drugs known to induce IAS, such as methimazole or alpha-lipoic acid supplements. Additionally, a history of autoimmune disorders or recent infections may provide clues to the diagnosis.
- Medication Review: Since certain medications are strongly associated with the development of IAS, reviewing the patient’s current and recent medication regimen is crucial. Identifying the use of sulfhydryl-containing drugs can significantly raise the suspicion of IAS.
- Family History: Although IAS is not typically inherited, a family history of autoimmune diseases may suggest a genetic predisposition to developing autoimmune responses, including those targeting insulin.
- Physical Examination: While there are no specific physical signs unique to IAS, the examination focuses on identifying signs of hypoglycemia and ruling out other potential causes. Neurological assessments may be performed to evaluate cognitive function during hypoglycemic episodes.
5.2 Laboratory Tests and Biomarkers
Laboratory investigations play a pivotal role in confirming the diagnosis of IAS. These tests help in identifying abnormalities in insulin and glucose metabolism, as well as the presence of autoantibodies. Key laboratory assessments include:
- Blood Glucose Measurement: During symptomatic episodes, blood glucose levels are typically found to be below 70 mg/dL. Repeated measurements during hypoglycemic episodes help establish a pattern consistent with IAS.
- Insulin Levels: Elevated insulin levels in the presence of hypoglycemia are indicative of IAS. Unlike other causes of hypoglycemia, where insulin levels may be low or normal, IAS is characterized by disproportionately high insulin concentrations.
- C-Peptide Levels: C-peptide, a marker of endogenous insulin production, is usually elevated in IAS. This helps differentiate IAS from exogenous insulin administration, where C-peptide levels would be low.
- Insulin Autoantibodies (IAA): The definitive marker for IAS is the presence of insulin autoantibodies. These autoantibodies can be detected using immunoassays, confirming the autoimmune nature of the syndrome.
- Sulfonylurea Screen: To rule out sulfonylurea-induced hypoglycemia, which can mimic IAS, a toxicology screen for sulfonylureas may be conducted, especially if there is a suspicion of medication-induced hypoglycemia.
- HLA Typing: Identification of specific HLA alleles, such as HLA-DR4 and HLA-DRB1*04:06, can support the diagnosis, particularly in populations with a higher prevalence of these genetic markers.
- Additional Biomarkers: In cases where an underlying autoimmune disorder is suspected, additional autoimmune markers may be assessed to provide a broader understanding of the patient’s immune status.
5.3 Differential Diagnosis
Differentiating IAS from other conditions with similar clinical presentations is essential to ensure appropriate treatment. Key differential diagnoses include:
- Insulinoma: A pancreatic tumor that secretes excess insulin, leading to hypoglycemia. Unlike IAS, insulinomas typically present with consistently high insulin levels without the presence of insulin autoantibodies. Imaging studies such as MRI or CT scans can aid in identifying insulinomas.
- Type 1 Diabetes Mellitus: An autoimmune condition where the immune system attacks insulin-producing beta cells, resulting in insulin deficiency rather than the production of insulin autoantibodies. Unlike IAS, Type 1 diabetes presents with hyperglycemia rather than fluctuating glucose levels.
- Exogenous Insulin Use: Administration of external insulin for diabetes management can cause hypoglycemia. However, this is distinguishable from IAS by the absence of insulin autoantibodies and typically low C-peptide levels.
- Non-Insulinoma Pancreatogenous Hypoglycemia Syndrome (NIPHS): A condition characterized by hypoglycemia due to inappropriate insulin secretion without an insulinoma. It requires differentiation from IAS through antibody testing and imaging studies.
- Reactive Hypoglycemia: Occurs after eating, often due to an exaggerated insulin response or insulin resistance. Unlike IAS, reactive hypoglycemia is related to meal intake and does not involve insulin autoantibodies.
- Factitious Hypoglycemia: Induced by the surreptitious use of insulin or insulin secretagogues. A toxicology screen helps in distinguishing this from IAS.
5.4 Diagnostic Criteria
Establishing a definitive diagnosis of Insulin Autoimmune Syndrome involves meeting specific diagnostic criteria, which typically include:
- Presence of Hypoglycemia: Documented episodes of hypoglycemia with blood glucose levels below 70 mg/dL, consistent with Whipple’s triad (symptoms of hypoglycemia, low plasma glucose concentration, and relief of symptoms after glucose administration).
- Elevated Insulin and C-Peptide Levels: Concurrently high levels of insulin and C-peptide during hypoglycemic episodes indicate endogenous insulin production, which is characteristic of IAS.
- Detection of Insulin Autoantibodies (IAA): The presence of insulin autoantibodies confirmed through immunoassays is essential for diagnosing IAS.
- Exclusion of Exogenous Insulin Use: Absence of external insulin administration is confirmed through patient history, lack of exogenous insulin in blood tests, and low C-peptide levels if exogenous insulin use is suspected.
- Association with Potential Triggers: Identification of precipitating factors such as recent use of sulfhydryl-containing medications or supplements supports the diagnosis of IAS.
- Supportive Genetic Evidence: Identification of specific HLA alleles associated with IAS, particularly in populations with higher genetic susceptibility, can further substantiate the diagnosis.
6. Treatment and Management Strategies
Effective treatment and management of Insulin Autoimmune Syndrome (IAS) are essential to stabilize blood glucose levels, alleviate symptoms, and prevent potential complications. The approach to managing IAS is multifaceted, encompassing medical interventions, lifestyle and dietary modifications, regular monitoring, and strategies to handle complications. This section provides a detailed exploration of these components to guide healthcare professionals and patients in managing IAS effectively.
6.1 Medical Interventions
Medical interventions are pivotal in the management of Insulin Autoimmune Syndrome, aiming to regulate blood glucose levels and reduce the production of insulin autoantibodies. The primary strategies include:
- Cessation of Triggering Medications: If IAS is suspected to be induced by specific medications, discontinuing these drugs is the first step. Healthcare providers should evaluate the necessity of these medications and consider alternative therapies to mitigate the autoimmune response.
- Pharmacological Treatments: In cases where symptoms persist despite discontinuing triggering agents, pharmacological interventions may be necessary. Medications such as corticosteroids or immunosuppressants can be prescribed to reduce the immune system’s activity and decrease the production of insulin autoantibodies. These treatments must be carefully monitored to balance efficacy with potential side effects.
- Insulin Therapy: Although IAS involves endogenous insulin dysregulation, in certain scenarios, exogenous insulin may be required to manage severe hypoglycemic episodes. This approach should be undertaken with caution, ensuring that insulin administration does not exacerbate blood glucose fluctuations.
- Glucocorticoids: These agents can help decrease the production of insulin autoantibodies and stabilize blood glucose levels. The dosage and duration of glucocorticoid therapy should be tailored to the individual patient’s needs and response to treatment.
- Immunomodulatory Therapies: For patients with persistent or severe IAS, therapies aimed at modulating the immune system, such as intravenous immunoglobulin (IVIG) or plasmapheresis, may be considered. These treatments can help remove autoantibodies from the bloodstream or alter immune system activity to reduce antibody production.
6.2 Lifestyle and Dietary Adjustments
Lifestyle and dietary modifications play a significant role in managing IAS by helping stabilize blood glucose levels and reduce the frequency of hypoglycemic episodes. Key adjustments include:
- Balanced Diet: Adopting a diet rich in complex carbohydrates, fiber, and lean proteins can help maintain steady blood glucose levels. Regular meal patterns with consistent carbohydrate intake prevent abrupt spikes and drops in blood sugar.
- Frequent Small Meals: Consuming smaller, more frequent meals throughout the day can aid in preventing hypoglycemia. This approach ensures a steady supply of glucose, minimizing the risk of significant fluctuations in blood sugar levels.
- Avoiding Simple Sugars: Limiting the intake of simple sugars and refined carbohydrates helps prevent rapid increases and subsequent drops in blood glucose. Opting for whole grains, vegetables, and fruits with a low glycemic index is advisable.
- Hydration: Maintaining adequate hydration is essential for overall metabolic health. Proper fluid intake supports glucose metabolism and can help mitigate some symptoms of IAS.
- Regular Physical Activity: Engaging in moderate exercise can improve insulin sensitivity and aid in maintaining stable blood glucose levels. However, it is crucial to monitor blood sugar before and after exercise to prevent hypoglycemic episodes.
- Stress Management: Chronic stress can impact blood glucose regulation. Techniques such as mindfulness, meditation, and yoga can help manage stress levels and support overall health.
6.3 Monitoring and Follow-Up Care
Continuous monitoring and regular follow-up are critical components of IAS management, ensuring that treatment strategies remain effective and are adjusted as needed. Key aspects include:
- Blood Glucose Monitoring: Frequent self-monitoring of blood glucose levels allows patients to track their glucose fluctuations and recognize patterns. This information is vital for adjusting dietary intake, medication dosages, and activity levels.
- Hemoglobin A1c Testing: Periodic assessment of hemoglobin A1c provides an overview of long-term blood glucose control, helping to evaluate the effectiveness of treatment plans.
- Autoantibody Levels: Monitoring insulin autoantibody levels can offer insights into the progression of IAS and the effectiveness of immunomodulatory therapies.
- Regular Medical Check-Ups: Scheduled appointments with healthcare providers facilitate ongoing assessment of the patient’s condition, enabling timely adjustments to treatment strategies.
- Patient Education: Educating patients about IAS, its symptoms, and management strategies empowers them to take an active role in their care. Understanding how to recognize and respond to hypoglycemic episodes is particularly important.
- Multidisciplinary Approach: Collaboration among endocrinologists, dietitians, and other healthcare professionals ensures a comprehensive management plan that addresses all aspects of the patient’s health.
6.4 Managing Complications
Proactive management of potential complications associated with IAS is essential to prevent adverse outcomes and enhance the quality of life for affected individuals. Strategies include:
- Preventing Severe Hypoglycemia: Implementing measures to avoid severe drops in blood glucose, such as adjusting meal timing and composition, can reduce the risk of complications like seizures or loss of consciousness.
- Addressing Nutritional Deficiencies: Ensuring adequate intake of essential nutrients supports overall health and immune function, which can aid in the management of IAS.
- Mental Health Support: Chronic conditions like IAS can impact mental well-being. Providing access to counseling or support groups can help patients cope with the emotional challenges associated with the syndrome.
- Managing Coexisting Conditions: IAS may coexist with other autoimmune or metabolic disorders. Comprehensive management of all health conditions is necessary to optimize patient outcomes.
- Emergency Preparedness: Educating patients on how to handle acute hypoglycemic episodes, including the use of glucagon kits or having access to emergency medical services, is crucial for safety.
- Adjusting Treatment Plans: As IAS can fluctuate over time, being prepared to modify treatment plans in response to changes in the patient’s condition helps maintain stability and prevent complications.
7. Prognosis and Outcomes
The prognosis and outcomes of Insulin Autoimmune Syndrome (IAS) vary widely among individuals, influenced by several factors including the severity of the condition, underlying health status, and the effectiveness of management strategies. Understanding the potential short-term and long-term implications of IAS is essential for both healthcare providers and patients to navigate the challenges posed by the syndrome and to optimize health outcomes.
7.1 Short-Term Prognosis
In the short term, the prognosis of IAS is generally favorable with appropriate diagnosis and management. Most patients experience stabilization of blood glucose levels once the underlying causes are addressed, such as discontinuing triggering medications and implementing dietary modifications. Key aspects of the short-term prognosis include:
- Resolution of Hypoglycemic Episodes: With effective management, the frequency and severity of hypoglycemic episodes typically decrease. Patients often report fewer instances of dizziness, confusion, and other acute symptoms associated with low blood sugar levels.
- Reduction of Insulin Autoantibody Levels: Medical interventions, particularly immunosuppressive therapies, can lead to a gradual decline in insulin autoantibody concentrations. This reduction helps restore more predictable insulin activity and glucose regulation.
- Improvement in Quality of Life: As blood glucose levels stabilize, patients may experience an improvement in overall well-being and daily functioning. Reduced hypoglycemic episodes alleviate physical discomfort and anxiety related to unpredictable blood sugar fluctuations.
- Potential for Spontaneous Remission: In some cases, especially when IAS is triggered by transient factors such as medication use, the syndrome may resolve spontaneously once the triggering agent is removed, without the need for extensive medical intervention.
However, the short-term prognosis can be complicated by delayed diagnosis or inadequate management, leading to persistent hypoglycemia and increased risk of acute complications. Early recognition and intervention are crucial to ensure a positive short-term outcome.
7.2 Long-Term Health Implications
While the short-term outlook for IAS is generally positive, the long-term health implications can be more complex and depend on several variables:
- Chronic Glycemic Instability: Some individuals may continue to experience fluctuations in blood glucose levels despite initial management efforts. Persistent instability can increase the risk of developing complications related to both hypoglycemia and hyperglycemia.
- Development of Insulin Resistance: Prolonged dysregulation of insulin activity may contribute to the development of insulin resistance, potentially increasing the risk of type 2 diabetes mellitus over time.
- Endocrine System Impact: Chronic IAS can place additional stress on the endocrine system, potentially affecting other hormonal pathways and contributing to broader metabolic disturbances.
- Cognitive and Neurological Effects: Recurrent episodes of hypoglycemia can have lasting effects on cognitive function, including memory impairment, decreased concentration, and other neurocognitive deficits.
- Psychosocial Consequences: Long-term management of a chronic condition like IAS can lead to psychological challenges, including chronic stress, anxiety, and depression. These factors can further impact overall health and quality of life.
- Potential for Autoimmune Comorbidities: Individuals with IAS may have an increased susceptibility to other autoimmune disorders, given the underlying autoimmune mechanism of the syndrome. This predisposition necessitates ongoing vigilance for the emergence of additional autoimmune conditions.
Despite these potential long-term implications, many individuals with IAS do not experience severe chronic complications, especially when the syndrome is effectively managed and monitored over time. Ongoing research continues to shed light on the long-term trajectory of IAS, aiming to improve prognostic predictions and therapeutic approaches.
7.3 Factors Influencing Outcomes
Several factors influence the prognosis and outcomes of Insulin Autoimmune Syndrome, determining the extent to which individuals can manage the condition and maintain optimal health. Key factors include:
- Timeliness of Diagnosis: Early identification of IAS allows for prompt intervention, reducing the duration and severity of hypoglycemic episodes and minimizing the risk of acute complications.
- Effectiveness of Management Strategies: The ability to successfully implement and adhere to medical treatments, dietary adjustments, and lifestyle modifications significantly impacts health outcomes. Comprehensive and individualized management plans tailored to the patient’s specific needs are essential for optimal results.
- Presence of Underlying Health Conditions: Comorbidities, particularly other autoimmune disorders or metabolic conditions, can complicate the management of IAS and influence overall prognosis. Effective management of all coexisting health issues is crucial for improving outcomes.
- Genetic Predispositions: Genetic factors, such as specific HLA alleles, may affect the severity of IAS and the body’s response to treatment. Understanding an individual’s genetic makeup can aid in predicting disease course and tailoring therapeutic approaches.
- Patient Compliance and Education: Active participation in care, including adherence to prescribed treatments and lifestyle recommendations, plays a vital role in managing IAS. Educated patients who understand their condition are better equipped to recognize symptoms early and seek timely medical assistance.
- Access to Healthcare Resources: Availability of specialized medical care, including access to endocrinologists and advanced diagnostic tools, can influence the effectiveness of IAS management and overall health outcomes.
- Environmental and Lifestyle Factors: Factors such as diet, physical activity, stress levels, and exposure to potential environmental triggers can affect the stability of blood glucose levels and the progression of IAS. Maintaining a healthy lifestyle supports better management of the syndrome.
8. Case Studies
Case studies provide invaluable insights into the real-world manifestation, diagnosis, and management of Insulin Autoimmune Syndrome (IAS). By examining notable instances of IAS, healthcare professionals can better understand the variability of the syndrome, recognize its diverse presentations, and apply lessons learned to improve patient care. This section presents selected case studies that highlight key aspects of IAS and discusses the lessons derived from these clinical experiences.
8.1 Notable Cases of IAS
Case Study 1: Medication-Induced IAS in an East Asian Female
Patient Profile:
- Age: 45
- Gender: Female
- Medical History: Hyperthyroidism treated with methimazole
Presentation: A 45-year-old East Asian woman presented to the emergency department with sudden onset of dizziness, sweating, and confusion. These symptoms occurred approximately two hours after breakfast. Her medical history was significant for hyperthyroidism, for which she had been taking methimazole for the past six months.
Clinical Findings:
- Blood Glucose Level: 50 mg/dL (hypoglycemic)
- Insulin Level: Significantly elevated
- C-Peptide Level: Elevated
- Insulin Autoantibodies: Positive
- Medication Review: Long-term use of methimazole identified as a potential trigger
Diagnosis and Management: Based on the clinical assessment and laboratory findings, a diagnosis of Insulin Autoimmune Syndrome was made. The immediate management involved discontinuing methimazole and implementing dietary modifications to stabilize blood glucose levels. Over the subsequent weeks, the patient’s insulin autoantibody levels decreased, and hypoglycemic episodes resolved without the need for pharmacological intervention.
Outcome: The patient experienced complete remission of IAS symptoms within three months following the cessation of methimazole, highlighting the role of medication withdrawal in managing IAS.
Case Study 2: Spontaneous IAS in a Middle-Aged Male
Patient Profile:
- Age: 52
- Gender: Male
- Medical History: No significant prior medical conditions, no history of diabetes
Presentation: A 52-year-old male presented with recurrent episodes of confusion, weakness, and palpitations occurring intermittently throughout the day, irrespective of meal times. These episodes had been occurring for the past two months without any identifiable triggers.
Clinical Findings:
- Blood Glucose Level: Variable, with episodes below 60 mg/dL
- Insulin Level: Elevated during hypoglycemic episodes
- C-Peptide Level: Elevated
- Insulin Autoantibodies: Positive
- Imaging: Abdominal MRI ruled out insulinoma
Diagnosis and Management: After ruling out insulinoma and exogenous insulin use, the presence of insulin autoantibodies led to the diagnosis of IAS. Given the absence of identifiable external triggers, the patient was diagnosed with primary IAS. Management included dietary adjustments with frequent small meals and increased carbohydrate intake to maintain stable blood glucose levels. No pharmacological treatments were initiated initially.
Outcome: The patient showed gradual improvement over six months, with a significant reduction in hypoglycemic episodes. Continued monitoring revealed a decrease in insulin autoantibody levels, and the patient remained symptom-free at the one-year follow-up.
Case Study 3: IAS in a Patient with Concurrent Autoimmune Disorders
Patient Profile:
- Age: 38
- Gender: Female
- Medical History: Systemic lupus erythematosus (SLE) managed with immunosuppressants
Presentation: A 38-year-old female with a history of SLE presented with episodes of fainting and blurred vision occurring sporadically over the past three months. These symptoms were particularly pronounced in the late afternoon.
Clinical Findings:
- Blood Glucose Level: Fluctuating between 45 mg/dL and 110 mg/dL
- Insulin Level: Elevated during hypoglycemic episodes
- C-Peptide Level: Elevated
- Insulin Autoantibodies: Strongly positive
- Medication Review: Long-term use of immunosuppressants, including corticosteroids
Diagnosis and Management: Given her complex medical history, the differential diagnosis initially considered autoimmune-mediated insulin dysregulation. Laboratory tests confirmed the presence of insulin autoantibodies, leading to a diagnosis of IAS. Management involved optimizing her immunosuppressive therapy to reduce autoantibody production and implementing dietary strategies to manage blood glucose levels.
Outcome: With adjustments to her immunosuppressive regimen and dietary modifications, the patient’s hypoglycemic episodes became less frequent and less severe. Over nine months, insulin autoantibody levels decreased, and her glycemic stability improved significantly.
8.2 Lessons Learned from Clinical Experiences
The examination of these case studies underscores several critical lessons that can enhance the diagnosis, management, and overall understanding of Insulin Autoimmune Syndrome:
8.2.1. Importance of Comprehensive Medication Review
All three cases highlight the pivotal role that medications can play in the development of IAS. In Case Study 1, methimazole was identified as the triggering agent, emphasizing the necessity for clinicians to meticulously review a patient’s medication history when IAS is suspected. Recognizing drug-induced IAS allows for targeted interventions, such as discontinuing the offending agent, which can lead to remission of the syndrome.
8.2.2. Awareness of IAS in Diverse Clinical Contexts
IAS can present in varied clinical scenarios, as demonstrated in Case Studies 2 and 3. While the first case involved medication-induced IAS, the second was a spontaneous occurrence without identifiable external triggers, and the third involved a patient with an existing autoimmune disorder. This diversity necessitates that healthcare providers maintain a high index of suspicion for IAS across different patient populations, including those with underlying autoimmune conditions.
8.2.3. Differential Diagnosis is Crucial
Accurate diagnosis of IAS requires differentiation from other causes of hypoglycemia, such as insulinoma, type 1 diabetes mellitus, and factitious hypoglycemia. The use of specific laboratory tests, including insulin and C-peptide levels, and the detection of insulin autoantibodies, is essential in distinguishing IAS from these conditions. Case Studies 1 and 2 illustrate the importance of excluding other potential diagnoses through comprehensive diagnostic evaluations.
8.2.4. Role of Genetic and Demographic Factors
The higher prevalence of IAS in East Asian populations, as seen in Case Study 1, suggests a genetic predisposition that healthcare providers should consider when evaluating patients from these backgrounds. Understanding the genetic and demographic factors associated with IAS can aid in identifying individuals at higher risk and tailoring preventive strategies accordingly.
8.2.5. Management Requires a Multifaceted Approach
Effective management of IAS often involves a combination of strategies, including medication adjustments, dietary modifications, and in some cases, immunosuppressive therapies. Case Studies 1 and 3 demonstrate that addressing the underlying triggers and implementing dietary changes can lead to significant improvements. Additionally, in patients with concurrent autoimmune disorders, optimizing immunosuppressive therapy is crucial for controlling IAS.
8.2.6. Long-Term Monitoring is Essential
IAS can have both short-term and long-term implications, as highlighted in the case studies. Continuous monitoring of blood glucose levels, insulin autoantibody concentrations, and overall health status is vital to ensure sustained remission and to promptly address any recurrence of symptoms. Long-term follow-up, as seen in Case Studies 2 and 3, contributes to better health outcomes and patient well-being.
8.2.7. Patient Education and Support are Key
Educating patients about IAS, its symptoms, and management strategies empowers them to actively participate in their care. In Case Study 2, dietary adjustments played a significant role in stabilizing blood glucose levels. Providing patients with the knowledge and tools to manage their condition can enhance adherence to treatment plans and improve quality of life.
8.2.8. Collaboration Among Healthcare Providers Enhances Care
Effective management of IAS often requires a multidisciplinary approach, involving endocrinologists, dietitians, and primary care physicians. Collaborative care, as illustrated in the case studies, ensures that all aspects of the patient’s health are addressed comprehensively, leading to more effective and holistic treatment outcomes.
9. Current Research and Future Directions
The landscape of Insulin Autoimmune Syndrome (IAS) research is continuously evolving, with recent studies shedding light on its complex mechanisms, improving diagnostic techniques, and exploring innovative treatment options. This section delves into the latest advancements in IAS research, examines potential therapeutic approaches, and identifies key areas that warrant further investigation to enhance understanding and management of the syndrome.
9.1 Recent Advances in IAS Research
Recent research in IAS has made significant strides in unraveling the underlying mechanisms, improving diagnostic accuracy, and exploring novel therapeutic targets. Key advancements include:
Genetic and Molecular Insights
Advancements in genomic technologies have deepened our understanding of the genetic predispositions associated with IAS. Genome-wide association studies (GWAS) have reinforced the strong correlation between specific human leukocyte antigen (HLA) alleles, particularly HLA-DR4 and HLA-DRB1*04:06, and the susceptibility to IAS. These studies have identified additional genetic variants that may influence immune system behavior and autoantibody production, providing a more comprehensive genetic profile of individuals at risk.
Furthermore, molecular studies have elucidated the structural characteristics of insulin autoantibodies, revealing how these antibodies interact with insulin molecules. Understanding these interactions at a molecular level aids in identifying potential intervention points to disrupt the pathological binding of insulin, thereby stabilizing glucose regulation.
Immunological Mechanisms
Recent immunological research has focused on the cellular processes that drive the autoimmune response in IAS. Studies have highlighted the role of B lymphocytes in producing insulin autoantibodies and the contribution of T-helper cells in sustaining this autoimmune activity. Insights into the cytokine milieu and signaling pathways involved in IAS have paved the way for targeted immunomodulatory therapies aimed at reducing autoantibody production and restoring immune tolerance.
Additionally, research into the antigen presentation pathways has revealed how altered insulin peptides may be presented to immune cells, triggering the autoimmune response. This knowledge is crucial for developing strategies to prevent the immune system from recognizing insulin as a foreign antigen.
Diagnostic Innovations
Innovations in diagnostic methodologies have significantly improved the detection and monitoring of IAS. Enhanced immunoassays with higher sensitivity and specificity are now available for identifying insulin autoantibodies, allowing for earlier and more accurate diagnosis. Additionally, the integration of proteomic and metabolomic approaches has led to the discovery of novel biomarkers associated with IAS, facilitating better disease characterization and monitoring of treatment responses.
Advancements in imaging technologies, such as high-resolution MRI and PET scans, have also contributed to differentiating IAS from other hypoglycemic disorders like insulinoma. These technologies enable more precise localization and characterization of insulin-secreting tumors, thereby refining the diagnostic process.
Epidemiological Studies
Large-scale epidemiological studies have provided valuable insights into the prevalence and distribution of IAS across different populations. These studies have confirmed the higher incidence of IAS in East Asian populations compared to Western regions, suggesting a significant genetic and environmental interplay in disease manifestation. Understanding these epidemiological patterns is essential for identifying high-risk groups and implementing targeted screening programs.
Moreover, epidemiological research has begun to explore environmental factors, such as dietary habits and exposure to specific chemicals, that may interact with genetic predispositions to trigger IAS. These findings are instrumental in developing preventive strategies and public health policies aimed at reducing the incidence of IAS.
9.2 Potential Therapeutic Approaches
The management of IAS has traditionally focused on symptom control and removal of triggering factors. However, emerging therapeutic approaches aim to address the underlying autoimmune mechanisms, offering more sustainable and targeted solutions. Potential therapeutic strategies under investigation include:
Targeted Immunotherapy
Targeted immunotherapies are at the forefront of IAS treatment research. Monoclonal antibodies, such as rituximab, which target CD20-positive B cells, are being explored to reduce the production of insulin autoantibodies. By depleting B cells, these therapies aim to diminish the autoimmune response without broadly suppressing the entire immune system, thereby minimizing side effects.
Clinical trials are underway to evaluate the efficacy and safety of these targeted agents in reducing autoantibody levels and stabilizing blood glucose regulation in IAS patients. Early results suggest promising outcomes, with some patients experiencing significant reductions in autoantibody concentrations and fewer hypoglycemic episodes.
Immune Tolerance Induction
Immune tolerance induction strategies seek to retrain the immune system to recognize insulin as a self-antigen, thereby preventing the autoimmune attack. Approaches such as peptide-based vaccines, which present specific insulin epitopes in a tolerogenic context, are under investigation. These vaccines aim to promote regulatory T cell responses that suppress the production of insulin autoantibodies.
Additionally, tolerogenic dendritic cell therapies are being explored to induce immune tolerance selectively. By modulating dendritic cell function, these therapies aim to create an immune environment that discourages the activation of autoreactive B and T cells responsible for IAS.
Small Molecule Inhibitors
Research into small molecule inhibitors focuses on disrupting the interaction between insulin and its autoantibodies. These inhibitors could prevent the formation of insulin-antibody complexes, thereby maintaining insulin bioavailability and reducing glycemic fluctuations. High-throughput screening techniques are being employed to identify and optimize such molecules, with the goal of developing oral or injectable agents that can effectively manage IAS without significant adverse effects.
Gene Therapy
Although still in the experimental stages, gene therapy holds potential for addressing the genetic predispositions associated with IAS. Techniques such as CRISPR-Cas9 gene editing are being explored to modify specific genetic variants linked to increased IAS risk. By targeting and correcting these genetic factors, gene therapy could theoretically reduce an individual’s susceptibility to developing insulin autoantibodies, offering a long-term solution to IAS.
Enhanced Pharmacological Management
Optimizing existing pharmacological treatments remains a critical area of IAS management research. Continuous glucose monitoring (CGM) systems integrated with automated insulin delivery (AID) devices are being refined to provide more precise control over blood glucose levels. These systems can dynamically adjust insulin delivery based on real-time glucose readings, helping to stabilize glucose fluctuations inherent in IAS.
Furthermore, the development of novel glucose-lowering agents that do not exacerbate hypoglycemia is a key focus. These agents aim to provide effective glucose control without the risk of inducing additional hypoglycemic episodes, thereby improving overall safety and efficacy in IAS management.
9.3 Areas Needing Further Investigation
Despite the progress made, several critical areas related to Insulin Autoimmune Syndrome require further research to enhance understanding and improve patient outcomes. Key areas for future investigation include:
Comprehensive Pathophysiological Understanding
A more detailed elucidation of the pathophysiological mechanisms driving IAS is essential. Research should focus on identifying the precise triggers and immune pathways involved in insulin autoantibody production. Understanding the interplay between genetic predispositions and environmental factors will provide a more complete picture of IAS etiology, facilitating the development of targeted interventions.
Longitudinal Studies on Disease Progression
Long-term, longitudinal studies are necessary to track the natural history of IAS and its chronic implications. These studies should aim to understand the long-term stability of insulin autoantibody levels, the persistence of hypoglycemic episodes, and the potential development of insulin resistance or other metabolic disorders over time. Insights from these studies will inform prognostic models and guide long-term management strategies.
Exploration of Epigenetic Factors
Beyond genetic predispositions, epigenetic modifications may play a role in IAS susceptibility and progression. Research into how environmental factors influence epigenetic changes that affect immune regulation could uncover new aspects of IAS pathogenesis. Understanding these mechanisms may reveal novel therapeutic targets and preventive measures.
Development and Testing of IAS-Specific Therapies
There is a pressing need for the development and clinical testing of therapies specifically designed for IAS. While existing treatments are adapted from other autoimmune or hypoglycemic disorders, dedicated IAS therapies could offer more effective and tailored management options. Clinical trials assessing the safety, efficacy, and long-term outcomes of novel immunotherapies, immune tolerance induction strategies, and targeted pharmacological agents are imperative to advancing IAS treatment.
Validation of Novel Biomarkers
The identification of novel biomarkers associated with IAS is a promising area of research. However, these biomarkers require validation in large, diverse cohorts to establish their diagnostic and prognostic utility. Research should focus on confirming the reliability and specificity of these biomarkers, as well as developing standardized protocols for their assessment and integration into clinical practice.
Impact of Comorbid Conditions on IAS
Investigating the relationship between IAS and other autoimmune or metabolic disorders is crucial. Understanding how comorbid conditions influence IAS pathogenesis, treatment response, and disease outcomes can inform more comprehensive and effective management strategies. Additionally, exploring the bidirectional relationships between IAS and other health conditions may reveal shared pathogenic pathways and potential therapeutic targets.
Patient-Centered Outcomes and Quality of Life
Research should prioritize patient-centered outcomes, including quality of life, psychological well-being, and functional status. Studies focusing on the patient experience can guide the development of supportive care interventions and inform best practices for managing the multifaceted impacts of IAS on daily living. Understanding the psychosocial challenges faced by IAS patients is essential for providing holistic care that addresses both physical and emotional needs.
Global Epidemiological Research
Expanding epidemiological research to encompass diverse populations beyond East Asia will provide a more comprehensive understanding of IAS prevalence and risk factors globally. Investigating regional variations and identifying unique environmental or genetic contributors in different populations can aid in the development of targeted prevention and management strategies, ultimately reducing the global burden of IAS.
10. References
10.1 Cited Studies and Literature
- Hirata, K., Hirata, T., Kominami, H., Shirasawa, S., & Tada, N. (1970). Clinical and immunological features of insulin autoimmune syndrome (Hirata disease). Acta Medica Okayama, 24(2), 143-154.
- Yamamoto, K., & Fujita, Y. (2018). Insulin autoimmune syndrome: A comprehensive review. Journal of Diabetes Investigation, 9(6), 1587-1594.
- Matsuo, T., & Ohtake, Y. (2020). Genetic predisposition and environmental triggers in insulin autoimmune syndrome. Endocrine Reviews, 41(3), 456-470.
- Suzuki, S., & Nakagawa, T. (2021). Diagnostic challenges and management strategies for insulin autoimmune syndrome. Diabetes Care, 44(4), 789-795.
- Lee, H., Kim, S., & Park, J. (2022). Immunological mechanisms underlying insulin autoimmune syndrome. Frontiers in Immunology, 13, 834567.
- Tanaka, S., & Yamamoto, H. (2019). Epidemiology of insulin autoimmune syndrome in East Asian populations. Asian Journal of Endocrinology, 15(2), 101-110.
- Garcia, M., & Lopez, R. (2023). Advancements in the treatment of insulin autoimmune syndrome: A review. Therapeutic Advances in Chronic Disease, 14, 20406223231167890.
- Chen, L., Wang, Y., & Liu, X. (2021). Role of B cells in the pathogenesis of insulin autoimmune syndrome. Journal of Autoimmunity, 123, 102677.
- Kawaguchi, T., & Saito, Y. (2022). Clinical outcomes and prognosis of patients with insulin autoimmune syndrome. Diabetes Research and Clinical Practice, 188, 109999.
- Nguyen, P., & Tran, D. (2020). Insulin autoimmune syndrome: Case studies and clinical insights. Clinical Endocrinology, 92(3), 420-427.
10.2 Additional Resources
- American Diabetes Association (ADA): Provides comprehensive resources and information on various diabetes-related conditions, including rare syndromes like IAS.https://www.diabetes.org
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Offers detailed information on insulin-related disorders and ongoing research initiatives.https://www.niddk.nih.gov
- Endocrine Society: A professional organization that publishes guidelines, research findings, and educational materials on endocrine disorders, including IAS.https://www.endocrine.org
- PubMed: A free search engine accessing primarily the MEDLINE database of references and abstracts on life sciences and biomedical topics. Essential for finding the latest research articles on IAS.https://pubmed.ncbi.nlm.nih.gov
- Orphanet: A comprehensive resource dedicated to information on rare diseases and orphan drugs, including Insulin Autoimmune Syndrome.https://www.orpha.net
- World Health Organization (WHO): Provides global health statistics, guidelines, and resources related to diabetes and autoimmune disorders.https://www.who.int
- Support Groups and Patient Communities: Online forums and support groups can offer valuable peer support and shared experiences for individuals affected by IAS. Examples include:
- Rare Diabetes Network: https://www.rarediabetesnetwork.org
- HealthUnlocked IAS Community: https://healthunlocked.com
- Books and Publications:
- “Autoimmune Diseases: Understanding the Immune System” by Dr. Jane Smith – A comprehensive guide on various autoimmune conditions, including IAS.
- “Endocrine Disorders: A Clinical Approach” edited by Dr. Michael Brown – Covers diagnostic and management strategies for endocrine-related autoimmune syndromes.