1. Introduction
High fasting insulin occurs when the level of insulin in the bloodstream remains elevated after a period of not eating—commonly eight to twelve hours. In some situations, this condition can be linked to autoimmune activity that disrupts normal processes within the body. The goal of this article is to provide a thorough overview of the background, potential causes, and possible effects of high fasting insulin connected to autoimmune responses. By adhering to recognized quality standards and E-E-A-T principles, we aim to offer a detailed perspective that helps individuals, healthcare providers, and policy makers understand the importance of proper diagnosis, management, and lifestyle interventions.
2. Definition of Fasting Insulin
General Explanation
- Measurement Timing: Fasting insulin is usually checked in the morning before any food intake.
- Significance: It offers an indication of the body’s insulin status without the impact of a recent meal. By evaluating fasting insulin, healthcare providers can spot early signs of insulin resistance or other metabolic irregularities.
Purpose of Insulin
- Hormone Production: Insulin is secreted by the beta cells in the pancreas.
- Regulation of Blood Sugar: Its primary function is to facilitate glucose uptake into cells, thus managing blood sugar levels.
- Metabolic Role: Insulin also influences fat storage and overall energy metabolism, making it a key player in maintaining stable blood glucose.
3. Autoimmune Factors
Immune System Response
- Autoimmune Activation: Autoimmune conditions occur when the body’s immune system mistakenly attacks its own cells or tissues.
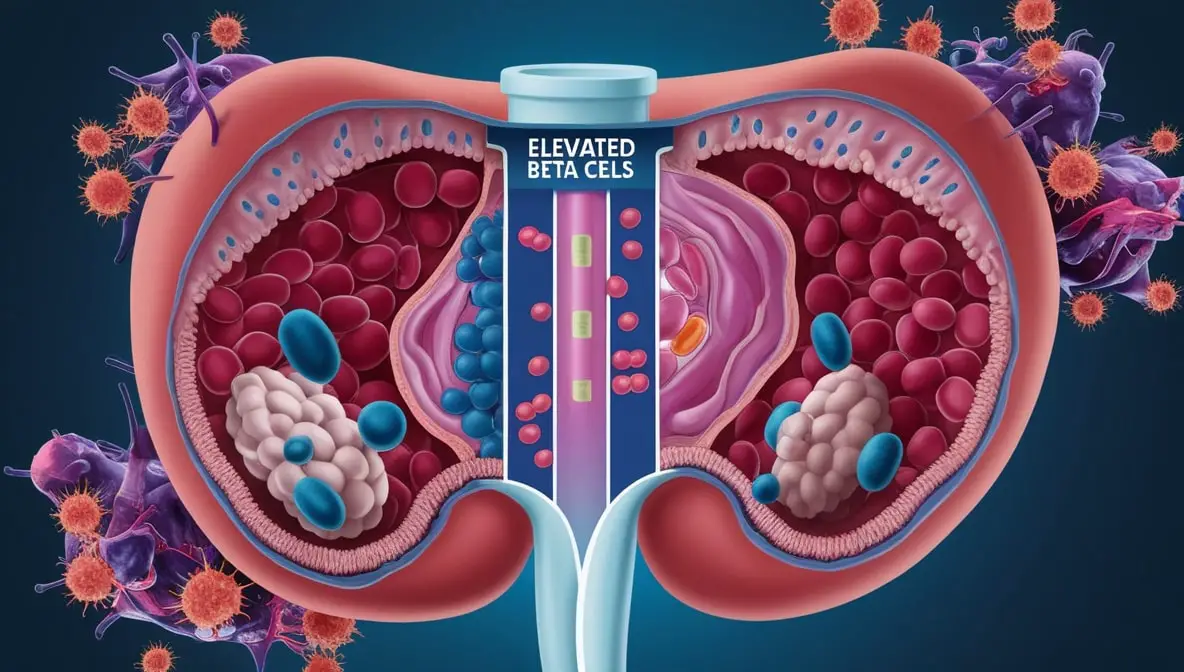
- Targeting the Pancreas: In the context of high fasting insulin, autoimmune activity may be directed toward the pancreas (including beta cells), or there could be systemic inflammation that impacts insulin effectiveness.
Possible Consequences
- Long-Term Inflammation: When chronic inflammation persists, it can disrupt insulin signaling pathways, fostering insulin resistance.
- Beta Cell Fluctuations: If immune cells target beta cells, insulin production may become inconsistent or abnormal, contributing to unstable blood sugar levels.
4. Contributing Factors
Inherited Predispositions
- Genetic Markers: Certain genetic markers can heighten susceptibility to autoimmune issues.
- Family History: Patterns of diabetes or autoimmune disorders within a family may indicate increased vulnerability for elevated fasting insulin.
Lifestyle Elements
- Physical Inactivity: Lack of regular exercise can intensify metabolic strain and worsen insulin resistance.
- Stress: Chronic stress triggers hormonal changes that may elevate blood sugar, fueling a cycle of increased insulin secretion.
- Sleep Patterns: Poor or irregular sleep can disrupt hormone balance and reduce insulin sensitivity.
Environmental Triggers
- Viruses and Toxins: Contact with specific pathogens or environmental toxins can spark inflammatory reactions that interfere with normal insulin function.
- Pollutants and Chronic Stress: Prolonged exposure to pollutants, as well as unrelenting stressors, can gradually amplify inflammatory pathways and put extra demands on insulin-regulating mechanisms.
5. Effects on Overall Health
Metabolic Impacts
- Precursor to Other Conditions: Elevated insulin levels over time increase the likelihood of insulin resistance and related complications (e.g., metabolic syndrome).
- Prediabetes and Diabetes Risk: Persistent hyperinsulinemia can lead to higher blood sugar levels, ultimately moving individuals closer to prediabetes or type 2 diabetes.
Organ Stress
- Pancreatic Strain: If the pancreas is consistently pushed to secrete high levels of insulin, beta cells may become fatigued, increasing the risk of impaired glucose control.
- Liver Function Changes: The liver, central to glucose regulation, may also experience dysfunction due to ongoing inflammation or insulin dysregulation.
6. Diagnostic Approaches
Laboratory Tests
- Fasting Insulin and Glucose: These tests offer an initial snapshot of how the body handles glucose and insulin without dietary influences.
- HbA1c: Reflects average blood glucose levels over the past three months.
- Inflammatory Markers: Tests such as C-reactive protein (CRP) or specific autoantibodies (e.g., anti-GAD antibodies) can uncover underlying immune-related activity.
Specialized Exams
- Imaging Studies: Ultrasound or MRI can sometimes reveal pancreatic inflammation or structural issues.
- Insulin Resistance Tests: The HOMA-IR (Homeostatic Model Assessment of Insulin Resistance) offers more detailed insight into how well the body uses insulin.
7. Dietary and Activity Guidelines
Nutritional Approaches
- Balanced Meals: Emphasize lean proteins, fibrous vegetables, whole grains, and healthy fats (like avocados, nuts, and olive oil).
- Limit Sugars and Refined Carbs: Reducing high-sugar beverages, candy, and ultra-processed foods helps stabilize insulin levels.
- Adequate Fiber: Consuming fruits, vegetables, and whole grains can improve insulin sensitivity and gut health.
Movement and Exercise
- Regular Physical Activity: Activities such as brisk walking, cycling, swimming, and resistance training (e.g., weightlifting) can enhance insulin sensitivity.
- Short Exercise Breaks: Even brief stretches or walks throughout the day may help sustain healthier blood sugar patterns.
Stress Reduction
- Impact of Chronic Stress: Ongoing stress can elevate cortisol, contributing to blood sugar fluctuations.
- Relaxation Techniques: Meditation, deep breathing exercises, or gentle yoga can help calm the nervous system and support immune balance.
8. Medical Interventions
Therapeutic Measures
- Medications: Depending on test results and health history, doctors might prescribe drugs that improve insulin sensitivity or regulate the immune system (e.g., metformin, certain immunomodulators).
- Individualized Care: Treatment plans vary, so working closely with healthcare providers—potentially including endocrinologists, immunologists, or dietitians—ensures a tailored approach.
Ongoing Monitoring
- Regular Checkups: Consistent evaluations of fasting insulin, glucose, and possibly inflammatory markers help track progress and adjust treatments.
- Early Detection of Complications: Routine visits and testing allow for timely interventions to address or prevent organ damage and related metabolic issues.
9. Practical Tips for Daily Life
Meal Planning
- Home-Cooked Meals: Controlling ingredients, portion sizes, and cooking methods is often easier at home.
- Structured Grocery Lists: Staying organized helps limit impulse buys that might spike insulin and glucose.
Physical Activity Routine
- Enjoyable Exercises: Whether it is dancing, swimming, or team sports, choosing activities you love fosters consistency.
- Accountability Tools: Using fitness trackers or scheduling workouts with friends can improve adherence to exercise routines.
Mind-Body Considerations
- Adequate Sleep: Setting regular bedtimes can help regulate hormones, including insulin and cortisol.
- Social Support: Connecting with family, friends, or support groups may relieve stress and bolster healthier habits.
10. Final Remarks
When high fasting insulin is coupled with autoimmune activity, addressing both metabolic and immunological components is crucial. While genetics can influence individual risk, lifestyle modifications—such as wholesome nutrition, consistent physical activity, and stress management—often have a powerful impact on insulin regulation. Ongoing monitoring and collaboration with healthcare professionals enable early detection of complications and personalized treatment adjustments. By remaining informed, practicing balanced self-care, and seeking medical guidance, many individuals can achieve healthier insulin levels and improve their overall metabolic well-being.
11. Refrences
- American Diabetes Association. Classification and diagnosis of diabetes: standards of medical care in diabetes—2023. Diabetes Care. 2023;46(Suppl 1):S19-S40. doi:10.2337/dc23-S002
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Insulin Resistance & Prediabetes. Accessed December 1, 2024. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance
- Centers for Disease Control and Prevention (CDC). National Diabetes Statistics Report, 2022. Published 2022. Accessed December 1, 2024. https://www.cdc.gov/diabetes/data/statistics-report/index.html
- Mayo Clinic. Autoimmune disease: Symptoms and causes. Updated August 9, 2022. Accessed December 1, 2024. https://www.mayoclinic.org/diseases-conditions/autoimmune-disease/symptoms-causes/syc-20351223
- World Health Organization (WHO). Diabetes. Updated June 16, 2022. Accessed December 1, 2024. https://www.who.int/news-room/fact-sheets/detail/diabetes
- DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979;237(3):E214-E223.
- Muniyappa R, Lee S, Chen H, Quon MJ. Current approaches for assessing insulin sensitivity and resistance in vivo: advantages, limitations, and appropriate usage. Am J Physiol Endocrinol Metab. 2008;294(1):E15-E26.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Autoimmune diseases. Accessed December 1, 2024. https://www.niddk.nih.gov/health-information/immune-diseases
Disclaimer
This article is provided for educational purposes only and should not be used as a replacement for personalized advice from a qualified healthcare provider. Always consult a physician or other appropriate health professional regarding any medical concerns or before making changes to your diet, exercise routine, or treatment plan.