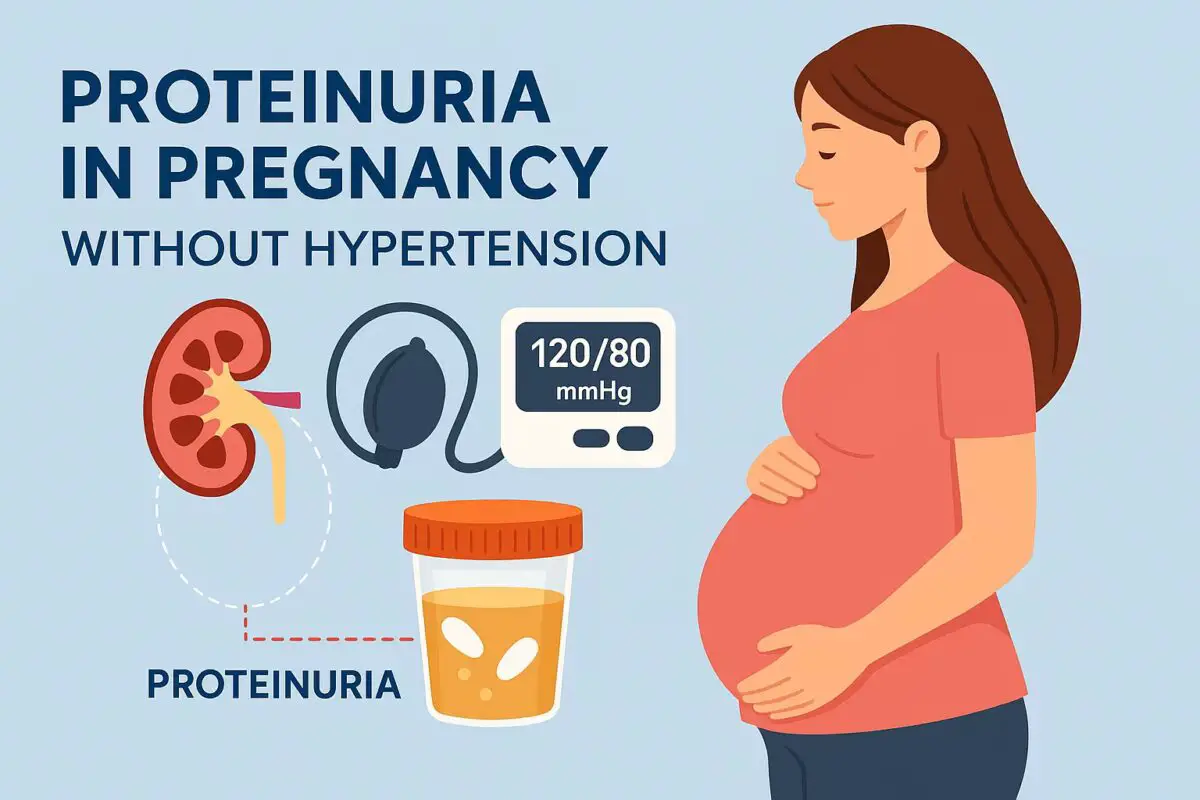
Preeclampsia is traditionally defined by high blood pressure during pregnancy combined with signs of organ stress, most commonly involving the kidneys, liver, or brain. Because hypertension is one of the hallmark warning signs, most pregnant women and even many clinicians automatically associate preeclampsia with elevated blood pressure readings. Yet a significant number of cases challenge the traditional definition. The question “Can you have preeclampsia without high blood pressure?” reveals a complex and evolving area of obstetric medicine.
Although high blood pressure is the classic diagnostic criterion, research shows that preeclampsia can develop quietly in its early stages, sometimes without an obvious rise in blood pressure. For some women, the first warning signs may appear in lab tests, symptoms, or fetal changes rather than in the blood pressure cuff. These atypical or “normotensive preeclampsia” cases require careful evaluation, because the absence of hypertension does not make the condition less dangerous.
Pregnancy is a time of profound physiological shifts, and the early vascular changes that lead to preeclampsia may begin long before symptoms appear. When these changes impact organs rather than systemic blood pressure, the condition can develop silently. Understanding how this happens helps expectant mothers recognize symptoms early and informs healthcare providers so they can intervene before the condition becomes life-threatening.
What Exactly Is Preeclampsia?
The Traditional Medical Definition
Preeclampsia is classified as a hypertensive disorder of pregnancy that typically occurs after 20 weeks of gestation. It involves high blood pressure combined with signs of organ dysfunction, most commonly elevated protein in the urine, abnormal liver enzymes, neurological symptoms, or platelet abnormalities. While hypertension forms the backbone of diagnosis, the condition affects far more than the cardiovascular system.
Historically, diagnostic criteria focused primarily on blood pressure measurements because they were easy to monitor and provided a clear marker of vascular stress. However, as modern research revealed deeper insights into the disorder’s pathophysiology, it became clear that preeclampsia is fundamentally a multi-system inflammatory and vascular disease rooted in placental dysfunction. This broader definition opens the door to recognizing cases where blood pressure is initially normal.
Not every pregnant woman fits textbook descriptions. Some develop symptoms such as severe headache or elevated liver enzymes in the absence of hypertension. Others may show signs of fetal growth restriction or placental abnormalities long before blood pressure rises. These cases challenge traditional expectations but are equally important to diagnose.
The Role of the Placenta in Preeclampsia Development
Preeclampsia begins in the placenta long before symptoms appear. Early in pregnancy, placental blood vessels must remodel to support increased blood flow to the fetus. In preeclampsia, this remodeling process is incomplete, leading to poor placental perfusion and oxidative stress. These problems trigger a release of inflammatory markers, anti-angiogenic factors, and cellular debris into the maternal bloodstream.
This cascade sets off widespread endothelial dysfunction, which is the root cause of preeclampsia symptoms. Endothelial cells are the inner lining of blood vessels; when they are damaged, organs lose their ability to regulate blood flow properly. The bloodstream becomes more prone to clotting, and the kidneys, liver, and brain experience increased stress.
These pathological changes can manifest in various ways. Some women first experience kidney-related signs such as protein in the urine, while others develop neurological symptoms like visual disturbances. Blood pressure elevation is common but not always the first symptom, especially in early or atypical forms of the disease.
Why Blood Pressure Alone Is Not Enough for Diagnosis
For decades, clinicians relied heavily on blood pressure as the primary warning sign of preeclampsia. But growing evidence shows that hypertension sometimes appears later in the disease process rather than early on. If elevated blood pressure is the only marker used, subtle but dangerous cases may go unnoticed.
Modern diagnostic criteria expand beyond hypertension to include organ dysfunction markers such as elevated liver enzymes, low platelets, kidney impairment, persistent headaches, visual changes, or pulmonary edema. These additional markers help identify preeclampsia before blood pressure rises or in cases where hypertension is mild or intermittent.
The shift toward broader diagnostic criteria underscores the complexity of the condition and helps protect mothers and babies by supporting earlier intervention. It also highlights the importance of understanding how preeclampsia can exist without high blood pressure.
Can You Have Preeclampsia Without High Blood Pressure?
Atypical or Normotensive Preeclampsia Explained
Yes, it is possible to have preeclampsia without high blood pressure. This form is known as normotensive preeclampsia or atypical preeclampsia. Although less common, it represents an important subset of cases that require careful monitoring and timely intervention.
Normotensive preeclampsia may present with symptoms such as proteinuria, upper abdominal pain, swelling, severe headaches, or abnormal lab values. Because blood pressure remains normal initially, these women may not be immediately recognized as having a serious condition. Timely diagnosis often depends on close clinical observation rather than routine blood pressure screening alone.
This type of preeclampsia may be related to placental dysfunction that primarily affects organ systems rather than systemic vascular pressure. Some women may have naturally lower blood pressure baselines, which can obscure early rises. Others may present with sudden and severe symptoms before hypertension develops.
Why Some Cases Occur Without Hypertension
The absence of hypertension in some preeclampsia cases is likely due to variations in how endothelial dysfunction affects different organ systems. In certain individuals, kidney impairment or liver inflammation may appear earlier than vascular pressure abnormalities. These changes may cause proteinuria, fluid retention, or neurological symptoms long before systemic hypertension sets in.
Additionally, preeclampsia is not a uniform disease. Genetic, immunological, and metabolic factors influence how symptoms arise. Some women may experience strong placental inflammation but minimal vascular resistance, preventing early blood pressure elevation. Others may compensate for vascular dysfunction longer due to healthy cardiovascular baselines or particular physiological adaptations.
These variations highlight why relying exclusively on blood pressure can delay diagnosis and underscore the importance of comprehensive prenatal screening.
How Common Is Preeclampsia Without High Blood Pressure?
Atypical or normotensive preeclampsia is relatively uncommon but not rare. Studies estimate that between 5% and 15% of preeclampsia cases may present without hypertension initially. The number varies depending on diagnostic criteria used, clinical monitoring frequency, and population-specific risk factors.
These cases appear more frequently in early-onset preeclampsia, where placental dysfunction begins early in pregnancy. They are also more common in individuals with autoimmune conditions, metabolic disorders, or certain genetic profiles. Because normotensive preeclampsia is harder to identify, it may be underdiagnosed, meaning the true rate could be slightly higher.
Recognizing this possibility is essential for clinicians and pregnant women alike. Awareness encourages attention to symptoms beyond blood pressure, supporting earlier detection and improved outcomes.
Symptoms of Preeclampsia Without High Blood Pressure
Organ Dysfunction as an Early Warning Sign
Preeclampsia affects multiple organ systems, and dysfunction in these areas can precede hypertension. Kidney impairment may cause proteinuria, reduced urine output, or fluid retention around the face, hands, or ankles. These signs may appear subtly, often mistaken for normal pregnancy swelling.
Liver dysfunction is another early sign. Women may experience tenderness beneath the right rib cage, nausea, vomiting, or abnormal liver enzymes in blood tests. These symptoms reflect hepatic stress rather than blood pressure elevation and can appear days or weeks before hypertension develops.
Because these organ systems play vital roles in maternal health, early dysfunction can lead to rapid deterioration if overlooked. Understanding these signs helps differentiate normal pregnancy symptoms from early pathology.
Neurological Symptoms and Visual Disturbances
Neurological symptoms are among the hallmark features of preeclampsia and can occur even when blood pressure is normal. Severe headaches, dizziness, ringing in the ears, blurred vision, or light sensitivity indicate neurological stress and vascular irritation. These symptoms may appear due to cerebral edema or changes in cerebral blood flow.
In some cases, neurological symptoms can escalate quickly, leading to migraine-like episodes, confusion, or seizures. These manifestations occur because preeclampsia affects blood vessel integrity throughout the body, including the brain. Blood pressure does not need to be elevated for neurological irritation to begin.
These symptoms always warrant immediate medical evaluation, particularly in the second half of pregnancy or postpartum.
Abnormal Lab Results and Silent Warning Signs
Blood tests often reveal preeclampsia before clinical symptoms appear. Elevated liver enzymes, low platelets, increased uric acid levels, and abnormal kidney function indicate developing pathology, regardless of blood pressure readings.
These lab abnormalities reflect inflammation, endothelial injury, or coagulation disturbances. Because they cannot be detected at home, regular prenatal care is essential for identifying changes early. A woman may feel entirely normal while lab values suggest significant risk.
The silent nature of these abnormalities underscores the importance of routine prenatal testing and emphasizes that preeclampsia can begin long before hypertension becomes evident.
Why Blood Pressure May Rise Late in Preeclampsia
The Progressive Nature of Vascular Dysfunction
Preeclampsia develops gradually for many women. Early endothelial dysfunction sets the stage long before blood pressure rises. The cardiovascular system may compensate for vascular stress initially, maintaining normal readings while internal damage progresses.
As the disease advances, endothelial injury accumulates, causing fluid imbalance, increased vascular resistance, and heightened inflammatory responses. These changes eventually overwhelm the cardiovascular system’s ability to maintain stability, causing blood pressure to rise abruptly.
This delayed onset explains why some women experience sudden and severe hypertension after days or weeks of normal readings.
Individual Variability in Vascular Adaptation
Not all pregnant women respond to placental dysfunction in the same way. Some have naturally low or stable baseline blood pressure and may remain normotensive longer. Others may have strong cardiovascular resilience or beneficial genetic traits that delay hypertension onset.
These variations complicate diagnosis because blood pressure alone cannot reliably predict disease severity. A woman with normal readings may still be at high risk if lab tests or physical symptoms point toward developing preeclampsia.
This highlights the importance of comprehensive evaluation rather than relying on a single parameter.
Why Blood Pressure Can Spike Suddenly
In some cases, hypertension may appear suddenly and dramatically. This is often seen in severe or late-onset preeclampsia. A woman may feel relatively normal and then experience a rapid spike in blood pressure within hours.
This sudden change reflects tipping points in vascular resistance, fluid retention, and inflammatory signaling. Rapid shifts require urgent medical attention because they increase the risk of placental abruption, stroke, and maternal seizure.
Understanding this possibility helps expectant mothers seek timely emergency care when late-appearing symptoms arise.
Risks of Undiagnosed Normotensive Preeclampsia
Maternal Complications
When preeclampsia goes undiagnosed due to absence of hypertension, mothers face increased risks of severe complications. Organ damage may progress silently, making sudden deterioration more likely. Liver failure, kidney impairment, or neurological symptoms can emerge rapidly once the disease escalates.
Women may also be at greater risk of developing HELLP syndrome, a dangerous variant of preeclampsia characterized by hemolysis, liver injury, and low platelets. HELLP syndrome frequently appears without severe hypertension, making it one of the most serious risks of normotensive preeclampsia.
Delayed diagnosis increases the risk of eclampsia, placental abruption, and postpartum complications. Early recognition remains essential for reducing morbidity.
Fetal Complications
The fetus is highly sensitive to changes in placental blood flow. Normotensive preeclampsia can lead to intrauterine growth restriction, reduced amniotic fluid, and decreased oxygen delivery long before symptoms appear in the mother.
Poor placental perfusion increases the risk of preterm birth, low birth weight, and fetal distress during labor. In severe cases, compromised placental function may lead to stillbirth if not recognized promptly.
Regular fetal monitoring, ultrasounds, and doppler studies help detect these issues early, improving neonatal outcomes.
Postpartum Risks
Preeclampsia can appear or worsen after delivery. Postpartum preeclampsia may present with headaches, elevated liver enzymes, or low platelets without hypertension initially. This delayed presentation increases the risk of stroke or seizure during the postpartum period.
Women recovering from childbirth may overlook these symptoms, mistaking them for normal postpartum fatigue. Awareness of atypical presentations helps prevent dangerous complications.
How Doctors Diagnose Preeclampsia Without High Blood Pressure
Emphasis on Lab Testing and Imaging
When blood pressure is normal, diagnosis relies heavily on laboratory data. Tests for proteinuria, liver enzymes, kidney function, platelet levels, and uric acid give critical insight into disease progression. These tests detect abnormalities invisible to blood pressure readings.
Ultrasound imaging may reveal placental insufficiency, fetal growth restriction, or reduced amniotic fluid. Doppler studies can identify abnormal blood flow patterns, supporting diagnosis even when clinical symptoms appear subtle.
These tools allow clinicians to identify early pathology before hypertension emerges.
Clinical History and Symptom Assessment
A thorough evaluation of symptoms is essential. Persistent headaches, visual disturbances, upper abdominal pain, nausea, swelling, or rapid weight gain provide valuable clues. Even when blood pressure remains normal, these symptoms suggest underlying endothelial and organ stress.
Doctors assess patterns rather than individual symptoms. For example, headaches accompanied by abnormal labs or right-sided abdominal pain may strongly indicate preeclampsia, regardless of blood pressure readings.
Symptom-based evaluation expands diagnostic accuracy and supports timely treatment.
Monitoring Trends Rather Than Single Values
Preeclampsia often evolves over time. Monitoring trends in symptoms, lab values, ultrasound results, and blood pressure helps clinicians identify concerning patterns. A slow rise in liver enzymes or gradual increase in proteinuria may signal early disease even if blood pressure is normal.
This trend-based approach allows earlier intervention and helps clinicians anticipate sudden escalations.
Treatment Options for Normotensive Preeclampsia
Close Monitoring and Frequent Testing
Treatment depends on disease severity and gestational age. In normotensive cases, doctors often begin with close monitoring, including frequent lab tests, physical assessments, and fetal evaluations. This helps detect early changes before they become dangerous.
Monitoring might occur weekly or more frequently when risks are high. Ultrasound evaluations help assess fetal wellbeing and growth, while maternal symptoms guide immediate decisions.
This careful observation ensures that both mother and baby remain safe as pregnancy progresses.
Medication and Symptom Management
Although blood pressure may not be elevated initially, medications may still be used to manage symptoms and reduce risks. Corticosteroids are often administered between 24 and 34 weeks gestation to accelerate fetal lung development in case early delivery becomes necessary.
Magnesium sulfate may be used to prevent seizures if neurological symptoms appear. This medication is standard in severe cases regardless of blood pressure status because it protects against eclampsia.
Symptom management supports maternal stability while allowing doctors to prolong pregnancy safely when possible.
Delivery as the Definitive Treatment
The only definitive cure for preeclampsia is delivery of the baby and placenta. When maternal or fetal risks become too great, doctors may recommend early induction or cesarean delivery, even if blood pressure remains normal.
Timing is critical. For mild cases, the goal is often to reach 37 weeks. For severe or rapidly progressing cases, earlier delivery may be necessary. Postpartum monitoring continues because symptoms can worsen temporarily.
Delivery resolves the underlying pathology, and most symptoms improve within days to weeks.
FAQs About Preeclampsia Without High Blood Pressure
Can you have preeclampsia if your blood pressure is normal?
Yes. Normotensive preeclampsia occurs when organ dysfunction appears before or without hypertension.
What are the early signs without high blood pressure?
Elevated liver enzymes, proteinuria, headaches, vision changes, or abdominal pain may appear first.
Is normotensive preeclampsia dangerous?
Yes. It carries the same risks as typical preeclampsia and requires urgent medical evaluation.
Can lab tests detect preeclampsia early?
Yes. Lab abnormalities often appear before blood pressure changes.
Does preeclampsia always involve swelling?
No. Swelling may occur but is not required for diagnosis.
Can preeclampsia begin after delivery?
Yes. Postpartum preeclampsia can develop with or without high blood pressure.
How is this type treated?
Monitoring, symptom management, medications, and delivery when risks increase.
Does every woman with normal blood pressure need testing?
Regular prenatal care ensures appropriate testing, even without hypertension.
Conclusion
Preeclampsia is a complex vascular and inflammatory disorder that can occur even without high blood pressure. Normotensive preeclampsia is less common but equally serious, requiring timely diagnosis and careful monitoring. Because early signs often appear in lab results, symptoms, or fetal assessments, pregnant women and clinicians must look beyond blood pressure alone. Understanding the atypical presentation of this condition empowers expectant mothers to seek early evaluation and ensures that serious complications can be prevented. With comprehensive prenatal care and appropriate medical intervention, both maternal and fetal outcomes can be significantly improved.
Disclaimer: This article is for educational purposes only and is not medical advice. Pregnant individuals experiencing symptoms or concerns should seek immediate evaluation from a qualified healthcare provider.