Managing your insulin dosage is key to controlling diabetes, whether you have Type 1 or Type 2 diabetes. Getting your insulin dose right helps keep your blood sugar levels stable, so you can avoid high blood sugar (hyperglycemia) and low blood sugar (hypoglycemia). This guide will walk you through everything you need to know—how to calculate your dose, how to use insulin dosage charts, and answer common questions. Let’s make insulin dosing easy to understand! 😊
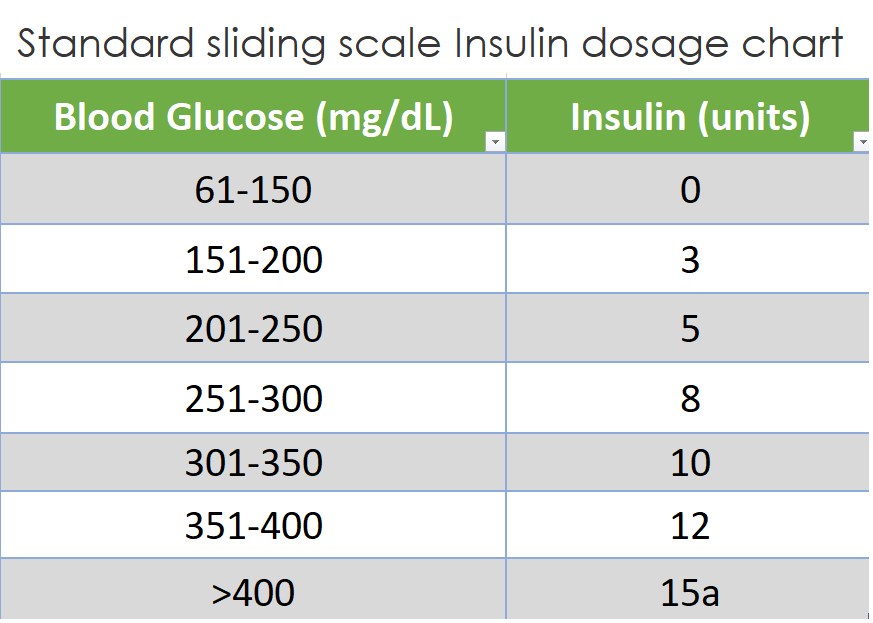
Standard Sliding Scale Insulin dosage chart
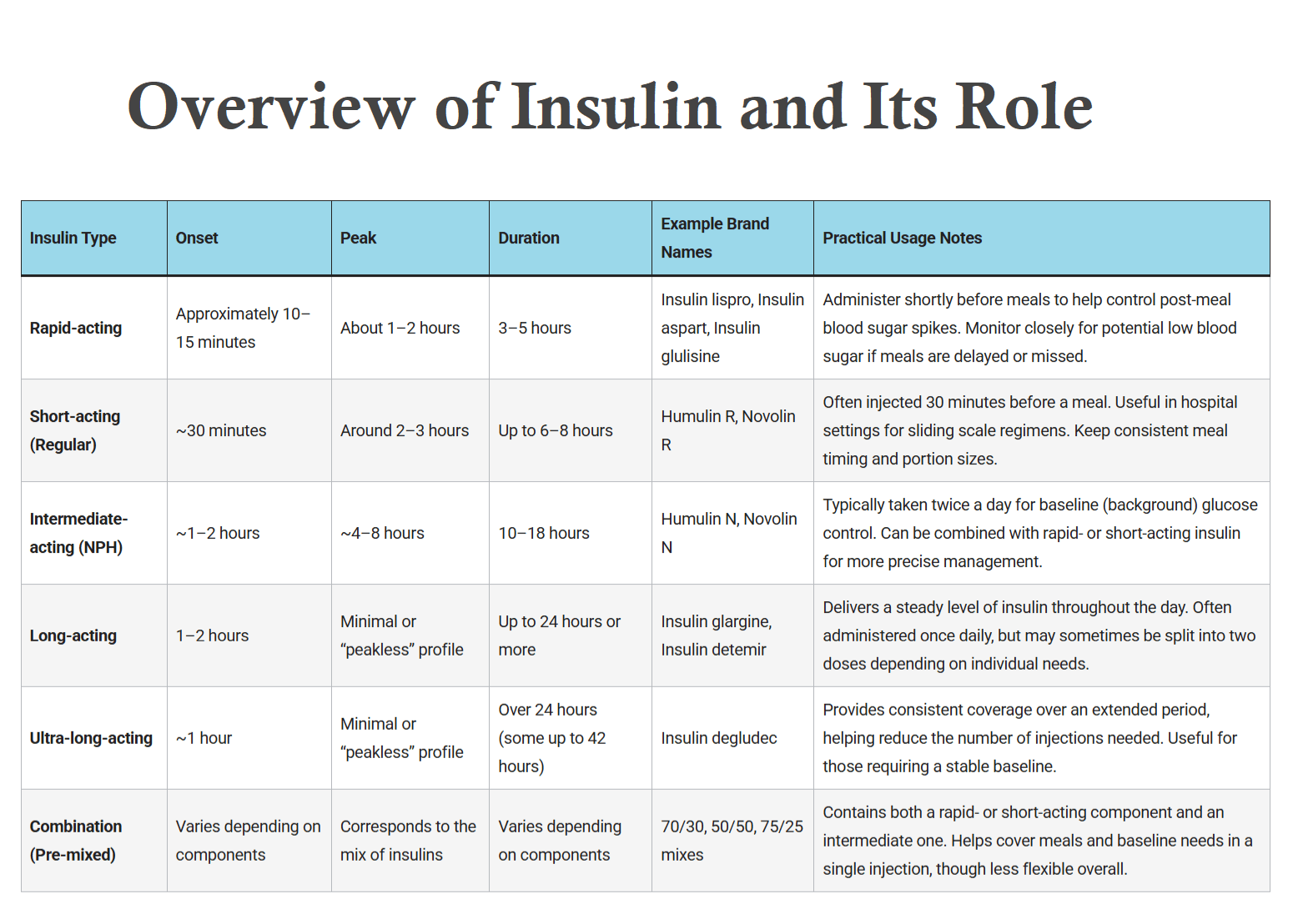
Insulin dosage is the amount of insulin you need to take to control your blood sugar. Getting the right dose depends on several factors, including:
- Your body weight
- Your current blood sugar levels
- How many carbohydrates you eat during meals
- Your activity level
- Your insulin sensitivity (how well your body uses insulin)
When you understand how to calculate and adjust your insulin dose, you can keep your blood sugar stable and avoid dangerous highs and lows.
How to Calculate Insulin Dosage

1. Basal Insulin Dosage
Basal insulin keeps your blood sugar level steady when you’re fasting (between meals and overnight). Here’s how to calculate it:
📝 Formula:
Basal insulin dose = 40-50% of your total daily insulin doseExample: If your total daily insulin need is 40 units, your basal insulin would be:
40 units × 50% = 20 units of basal insulinThis insulin is usually injected once daily in the morning or evening, but your doctor may adjust the timing based on your needs.
2. Bolus Insulin Dosage (Carb Coverage)
Bolus insulin helps cover the rise in blood sugar that happens after you eat. The bolus insulin dose depends on how many carbs you eat and your insulin-to-carb ratio.
📝 Formula:
Bolus insulin dose = Total grams of carbs ÷ Insulin-to-carb ratioExample: If you’re eating a meal with 60 grams of carbs and your insulin-to-carb ratio is 1:10 (1 unit of insulin for every 10 grams of carbs):
60 grams ÷ 10 = 6 units of bolus insulinThis means you’ll need 6 units of rapid-acting insulin to cover the carbs in your meal.
3. Blood Sugar Correction Dose (For High Blood Sugar)
If your blood sugar is high before a meal, you may need extra insulin to bring it down to your target level. This is called a correction dose.
📝 Formula:
Correction dose = (Current blood sugar – Target blood sugar) ÷ Correction factorExample: If your current blood sugar is 220 mg/dL, your target blood sugar is 120 mg/dL, and your correction factor is 50 mg/dL per unit of insulin:
(220 - 120) ÷ 50 = 2 units of insulinSo, you’d need to add 2 units to your bolus insulin to bring your blood sugar down to target.
Insulin Dosage Chart for Type 1 and Type 2 Diabetes
To make things easier, here are insulin dosage charts for Type 1 and Type 2 diabetes. These charts help guide how much insulin to take based on your carbohydrate intake or blood sugar levels.
1. Insulin Dosage Chart for Blood Sugar Correction
| Blood Sugar (mg/dL) | Correction Insulin Units |
|---|---|
| 120-170 | 1 unit |
| 170-220 | 2 units |
| 220-270 | 3 units |
| 270-300 | 4 units |
| Above 300 | Contact your doctor |
2. Insulin Dosage Chart for Carbohydrate Coverage (Bolus Insulin)

| Carbohydrates in Meal (g) | Rapid-Acting Insulin Units |
|---|---|
| 0-15 | 1 unit |
| 16-30 | 2 units |
| 31-45 | 3 units |
| 46-60 | 4 units |
These charts are a simple guide to help you adjust your insulin based on your food and blood sugar.
What Is the Average Dose of Insulin for Type 2 Diabetes?
For people with Type 2 diabetes, insulin resistance usually means you’ll need higher doses of insulin. The average starting dose is typically around:
0.1 to 0.2 units of insulin per kilogram (kg) of body weight per day.For example, if you weigh 70 kg, your starting daily insulin dose might be:
0.2 units × 70 kg = 14 units per dayYour doctor will adjust the dosage based on how well your blood sugar is controlled over time.
Is 20 Units of Insulin a Lot?
Not necessarily! For many people with Type 2 diabetes, 20 units of insulin is a normal dose. Depending on how resistant your body is to insulin, some people might need 20-50 units per day. Others with more severe insulin resistance may require more.
Always work with your healthcare provider to determine the right dose for you.
Maximum Insulin Dose Per Day
There is no exact “maximum” insulin dose, but typically, doses above 100 units per day are considered high and need close monitoring. People with severe insulin resistance may need doses higher than 100 units. Always consult your doctor to make sure you’re getting the right amount.
Insulin Dosage by Weight (Insulin Dose per kg)
A common way to calculate your insulin dose is based on your body weight. This method is particularly helpful when you’re first starting insulin therapy.
📝 Formula:
Total daily insulin (units) = 0.55 × Body weight (kg)Example: If you weigh 80 kg, your total daily insulin dose would be:
0.55 × 80 = 44 units of insulin per dayThis daily dose is split between basal insulin (40-50%) and bolus insulin (50-60%), depending on your meals and blood sugar patterns.
Insulin Dosage Chart for Type 1 Diabetes
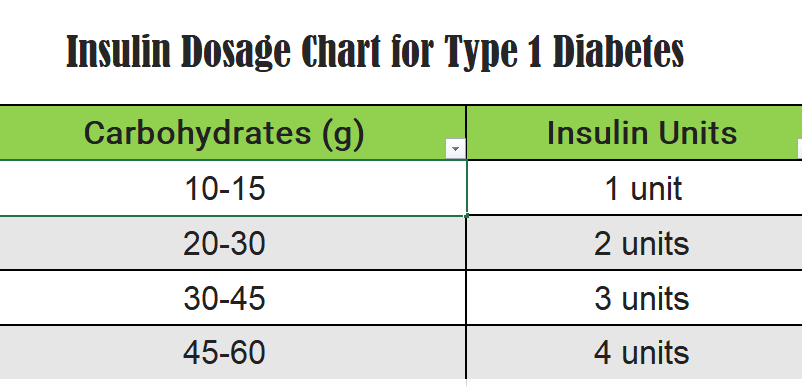
For people with Type 1 diabetes, insulin therapy is essential for survival. Here’s a simple chart showing how much rapid-acting insulin is typically needed based on the number of carbohydrates you eat:
| Carbohydrates (g) | Insulin Units |
|---|---|
| 10-15 | 1 unit |
| 20-30 | 2 units |
| 30-45 | 3 units |
| 45-60 | 4 units |
Insulin Formulas for Dosing: Detailed Breakdown
Here are the key formulas you’ll need to calculate your insulin dosage:
1. Carbohydrate Coverage Formula (Bolus Insulin for Meals)
Bolus insulin dose = Total grams of carbs ÷ Insulin-to-carb ratioExample: If you’re eating 60 grams of carbs and your insulin-to-carb ratio is 1:10:
60 grams ÷ 10 = 6 units of insulin2. Blood Sugar Correction Formula
Correction dose = (Current blood sugar – Target blood sugar) ÷ Correction factorExample: If your blood sugar is 220 mg/dL
, your target is 120 mg/dL, and your correction factor is 50:
(220 – 120) ÷ 50 = 2 units of insulin3. Basal Insulin Formula
Basal insulin dose = 40-50% of your total daily insulinExample: If your total daily insulin need is 50 units, your basal insulin dose would be:
50 units × 50% = 25 units of basal insulin4. Total Daily Insulin Formula
Total daily insulin (units) = 0.55 × Body weight (kg)Example: If you weigh 80 kg, your total insulin dose would be:
0.55 × 80 = 44 units of insulin per dayFinal Tips for Managing Insulin Dosage
- Monitor your blood sugar: Check your levels regularly and adjust your dose based on your results.
- Know your carbs: Keep track of how many carbs you eat so you can adjust your bolus insulin correctly.
- Stay active: Exercise helps lower blood sugar naturally, which means you might need less insulin when you work out. 🏋️♂️
- Consult your doctor: Your insulin needs can change, so always check with your doctor if you’re unsure about your dose.
FAQs About Insulin Dosage
To calculate your insulin dosage, you can use the formula 0.55 units of insulin per kg of body weight for your total daily dose. Split this dose between basal and bolus insulin based on your meals and blood sugar levels.
No, 20 units of insulin is a common dose for people with Type 2 diabetes. Your actual dosage will depend on your insulin sensitivity and how well your blood sugar is controlled.
There is no set maximum dose, but doses above 100 units per day are considered high and should be carefully monitored by a healthcare provider. In some cases, people with insulin resistance may require more.
You’ll need to adjust your insulin dose based on your blood sugar levels. If your blood sugar is consistently high or low, consult with your doctor to change your dosage.
Not taking enough insulin can result in high blood sugar (hyperglycemia), which can lead to diabetic ketoacidosis (DKA) in people with Type 1 diabetes, a dangerous condition that can be life-threatening.
Resuorces:
1. MDApp – Insulin Dosage Calculator
- Offers a detailed calculator for both carbohydrate coverage and high blood sugar correction, making it easier to estimate daily insulin needs.
- Visit MDApp【35†source】
2. University of California, San Francisco (UCSF) – Calculating Insulin Doses
- Comprehensive instructions for calculating both basal and bolus insulin doses, with examples for different types of diabetes.
- Visit UCSF【36†source】
3. American Academy of Family Physicians (AAFP) – Outpatient Insulin Management for Type 2 Diabetes
- Offers guidelines on insulin titration, basal-bolus therapy, and adjustment schedules for Type 2 diabetes.
- Visit AAFP【37†source】
4. Diabetes Teaching Center (UCSF) – Calculating Total Daily Insulin Dose
- This resource explains how to calculate the total daily insulin requirement based on body weight and insulin sensitivity.
- Visit UCSF【36†source】
These trusted resources will give you a deeper understanding of insulin dosing calculations and management techniques.